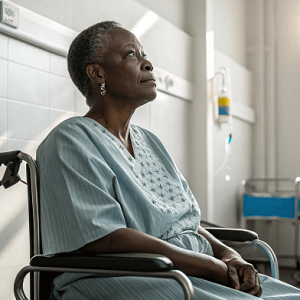
Survival outcomes for uterine cancer in the United States reveal stark and persistent racial and ethnic disparities, as reported in a recent cohort study analyzing data between 2000 and 2019. Researchers examined how race and ethnicity are associated with survival rates after a uterine cancer diagnosis, factoring in where people live and the diversity of their communities.
Findings demonstrate that Black women consistently experience worse survival rates compared with White women in almost all regions. Asian and Hispanic women, on the other hand, often show better survival rates than their White counterparts, but this advantage is not uniform across the country. The study highlights that disparities are present in multiple counties and not limited to just one area or state, reflecting a widespread issue.
These differences in survival are not strictly due to biological factors but seem deeply intertwined with social, environmental, and systemic issues. Racial and ethnic minority groups are impacted by factors ranging from access to care, variation in cancer treatment, and broader socioeconomic conditions that shape health outcomes. Minority communities continue to face obstacles including limitations in health resources and possible delays in diagnosis and treatment.
Researchers call attention to the need for targeted interventions, emphasizing that efforts to reduce these disparities must consider local contexts and the diverse experiences of different population groups. Addressing health disparities demands a multifaceted approach, acknowledging the variety of forces driving unequal outcomes in uterine cancer survival across America.
See “Geographic Variation of Racial and Ethnic Differences in Uterine Cancer Survival” (April 25, 2025)