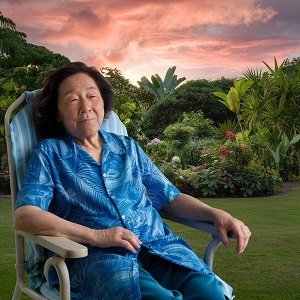
A recent study has uncovered significant racial disparities in the prevalence of cardiometabolic disorders among Alzheimer’s disease patients, with Native Hawaiians and Pacific Islanders (NHPI) facing disproportionately higher risks. The research, conducted using data from the National Inpatient Sample database, reveals a concerning trend in healthcare outcomes for these minority communities.
The study found that NHPI patients with Alzheimer’s disease had higher rates of several cardiometabolic disorders compared to their white counterparts. Notably, NHPI patients showed significantly higher odds of having hypertension, diabetes with complications, and obesity. These findings highlight the complex interplay between racial background, Alzheimer’s disease, and cardiovascular health.
Researchers observed that NHPI patients were 2.4 times more likely to have hypertension and 2.8 times more likely to have diabetes with complications compared to white patients. The disparity was even more pronounced for obesity, with NHPI patients being 3.4 times more likely to be affected.
These disparities persisted even after adjusting for various demographic and socioeconomic factors, suggesting deep-rooted systemic issues in healthcare delivery and access for NHPI communities. The study’s authors emphasize the need for targeted interventions and culturally sensitive healthcare approaches to address these disparities.
The findings underscore the importance of considering racial and ethnic backgrounds in the management of Alzheimer’s disease and associated comorbidities. As the population ages and the prevalence of Alzheimer’s disease increases, addressing these health disparities becomes crucial for ensuring equitable healthcare outcomes for all communities.
See: “Racial Disparities in Cardiometabolic Disorders Among Alzheimer’s Disease Patients: A Study on Native Hawaiians and Pacific Islanders” (December 24, 2024)