Flooding from hurricanes brings lasting health threats for older adults, notably in disadvantaged and minority communities across New York, New Jersey, and Connecticut. A major cohort study tracking Medicare beneficiaries over five years found “hurricane-related flooding was associated with increases in cardiovascular disease (CVD) event rates as long as 5 years after landfall.” The greatest spike was seen in heart failure risk, especially for residents in New Jersey.
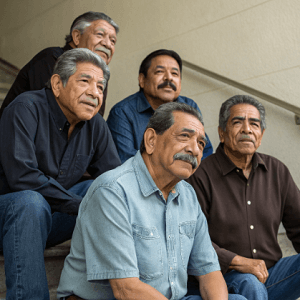
Researchers observed that zip codes most affected by flooding had lower median household incomes and a sharply higher proportion of Hispanic residents. The study concluded that “adverse health outcomes related to hurricane impacts have been well characterized among racial and ethnic minoritized populations,” and noted that disaster recovery policies typically focus too narrowly on emergency care in the months after landfall. A more persistent, place-based vulnerability remains, impacting health long after the news crews leave.
These findings spotlight the amplifying effects of social deprivation in the aftermath of natural disasters—including barriers to long-term follow-up care and rising chronic disease rates. Experts highlight the need to address disaster management frameworks “to consider and address long-term effects of hurricane exposure beyond simply the prioritization of emergency care.”
The study urges clinicians and policymakers to develop plans that protect those most exposed and disadvantaged, building resilience against a cascade of health risks accelerated by extreme weather.
See: “Hurricane Exposure and Risk of Long-Term Cardiovascular Disease Outcomes” (September 3, 2025)