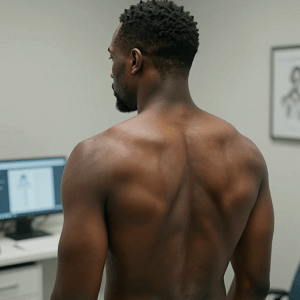
For many patients of color, a visit to the dermatologist can mean entering a system that was never designed with their skin in mind. At the European Academy of Dermatology and Venereology Congress, experts warned that long‑standing gaps in dermatologic training continue to fuel dangerous delays in diagnosis for people with darker skin.
Ophelia Entsir Dadzie noted that dermatology’s pattern‑recognition tools were built on observations in light‑skinned patients. She described a case in which a Black man with facial swelling and nodules was initially evaluated for infections such as leprosy or tuberculosis. Only a biopsy revealed a granulomatous reaction to fillers. The treating physician insisted, “But he cannot have had fillers; he is Black!”—a moment that captured how bias can derail care.
Dadzie urged clinicians to “assess the patients and their skin conditions holistically,” emphasizing that hyperpigmented lesions often signal active inflammation, not late‑stage disease. She also highlighted conditions like facial Afro‑Caribbean childhood eruption that are frequently overlooked in darker skin.
Cancer detection poses an even more serious threat. Ibrahima Traoré explained that melanomas in dark skin are often found late because of a “false sense of security” and because they tend to appear on acral or mucosal sites. Subtle pigment changes can be missed, and some cancers mimic benign inflammatory lesions. Traoré advised lowering the threshold for biopsy and expanding the ABCDE rule to include acral, mucosal, and amelanotic presentations.
Experts agreed that without targeted training and updated diagnostic tools, people with dark skin will continue to face preventable disparities in dermatologic care.
See: “Is Dark Skin the Blind Spot of Dermatology?” (December 05, 2025)