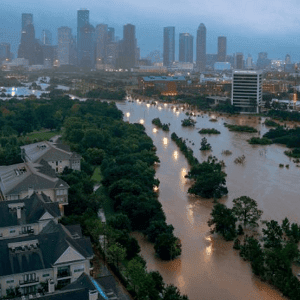
When Hurricane Harvey swept through Texas and Louisiana in 2017, the official death count stood at 103. But a new University of Michigan study reveals the storm’s true human cost was far grimmer, with an estimated 3,738 additional deaths among older adults in the year following the disaster.
The research exposes stark racial disparities in who survived Harvey’s aftermath. Black older adults faced a 6% higher risk of death in the year after the storm, while Hispanic and Latino populations experienced an alarming 13% increase in mortality risk compared to other groups.
Lead author Sue Anne Bell, a nursing professor at the University of Michigan, explains that disasters expose and magnify underlying fragilities in health systems. For older adults requiring regular medical care, even temporary disruptions can prove fatal.
The study examined Medicare data from nearly 1.8 million beneficiaries aged 65 and older, tracking their health outcomes before and after Harvey. Researchers found that older adults exposed to heavy rainfall faced a 3% increased death risk within the following year.
Those with chronic conditions suffered most severely. Patients with Alzheimer’s disease and related dementias accounted for 1,245 deaths—a 5% higher mortality risk. Chronic kidney disease patients faced 423 attributable deaths, while diabetes patients also experienced a 4% elevated death risk.
The findings underscore how severe weather events disproportionately harm vulnerable populations, particularly minority communities who already face systemic healthcare barriers. As climate disasters intensify, these disparities demand urgent attention.
See: “Severe Weather Is Deadly for Vulnerable Older Adults Long After the Storm Ends, Study Finds” (January 14, 2026)