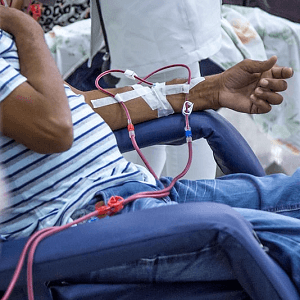
A new study reveals alarming racial disparities in deaths from obesity-related chronic kidney disease (CKD) among U.S. adults. Between 2018 and 2023, mortality rates climbed from 0.27 to 0.36 per 100,000, peaking in 2021. While men had slightly higher rates than women, the most striking differences were seen across racial lines.
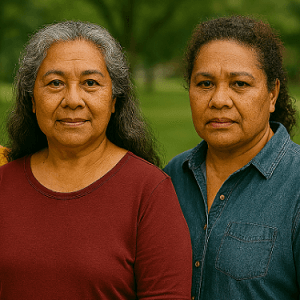
Native Hawaiian and Other Pacific Islander adults faced the highest age-adjusted mortality rate (AAMR) at 1.27 per 100,000, followed by Black or African American adults at 0.66. In contrast, Asian adults had the lowest rate at just 0.06. White adults had an AAMR of 0.38, underscoring the disproportionate burden on minority communities.
“Non-Hispanic Blacks showed the highest AAMRs among all the studied races,” the authors reported. They pointed to biological, social, and genetic factors—including APOL1 risk alleles—as possible contributors to faster disease progression in Black populations. Structural and socioeconomic disparities also play a role, with Black Americans more likely to suffer from obesity and less likely to access timely treatment.
Geographic disparities were also evident. Southern and Midwestern states, including Oklahoma and South Carolina, had the highest mortality rates, while Northeastern states like New York and Massachusetts reported the lowest.
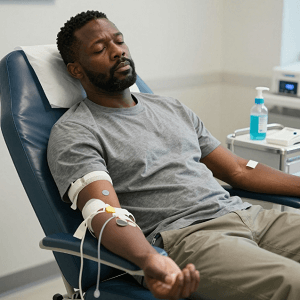
The study calls for targeted public health interventions, emphasizing early CKD screening and equitable access to treatment in high-risk populations. Without action, the mortality gap may continue to widen, leaving minority communities disproportionately affected by this preventable disease.
See: “Demographic Disparities in Mortality Trends of Obesity-Related Chronic Kidney Disease Among Adults in the United States From 2018 to 2023” (October 24, 2025)