Disparity Disruptors


Native Hawaiians, Pacific Islanders Face highest risk of ischemic stroke in the US
A new study has revealed that Native Hawaiian and Pacific Islander communities face the highest risk of ischemic stroke in the United States—far surpassing other racial and ethnic groups. The study, led by Dr. Fadar O. Otite and published in Neurology, analyzed six years of hospital data from Florida, Georgia, Maryland, and New York. The findings are stark: Native Hawaiian and Pacific Islanders experienced 591 strokes per 100,000 people. That’s more than double the rate for Black individuals (292), over three times the rate for white individuals (180), and nearly six times the rate for Asian individuals (108). Even after adjusting for hospitalization length and medical advances, the disparities remained. “These findings also lend support to the need for parsing out information on race and ethnicity in health care databases,” said Otite, noting that Asian and Pacific Islander populations are often grouped together, masking critical differences. Geographic variation added another layer to the disparity. In Florida, Native Hawaiian and Pacific Islanders had lower stroke rates than Black individuals, but in Georgia, Maryland, and New York, their rates were higher. Researchers suggest this may reflect differences in healthcare access or region-specific health risks. The study underscores the urgent need for more targeted research and public health interventions. As Otite emphasized, Native Hawaiian and Pacific Islanders are among the fastest-growing populations in the U.S. and already face high rates of cardiovascular disease. See: “Native Hawaiian and Pacific Islanders face highest stroke risk” (September 2, 2025)
Post Template
Black women in the United States are dying during pregnancy and childbirth at alarming rates—two to four times higher than White, Hispanic, or Asian women. A new analysis from the McKinsey Institute for Economic Mobility and the McKinsey Health Institute reports that maternal mortality among Black women reached 50 deaths per 100,000 live births in 2023, and could nearly double by 2040 if current trends persist. Beyond mortality, Black women face disproportionate rates of serious conditions such as preeclampsia, gestational diabetes, and postpartum depression. These health challenges may not always be fatal, but they take a heavy toll. The report estimates that in 2025 alone, Black women giving birth will lose 350,000 healthy life years to disability and illness tied to maternal health. The disparities extend to infants. Black babies are more than twice as likely as their White, Hispanic, and Asian peers to die before their first birthday. Complications like preterm birth, low birth weight, and limited access to prenatal care are driving factors. Closing this gap could save 35,000 Black infants by 2040. The report also highlights broader costs. Maternal-health inequities not only devastate families but weaken the economy. Addressing the crisis could restore healthy years of life, save billions in healthcare spending, and add $24.4 billion to U.S. GDP through improved workforce participation. Underlying these disparities are structural drivers, including racism in healthcare, chronic disease burdens, and higher allostatic load—a biological marker of stress that shortens life and raises risks of hypertension, diabetes, and heart disease. See: “Closing the Black maternal-health gap: Healthier lives, stronger economies” (August 13, 2025)

Latino leaders launch health institute to fight research cuts
In response to sweeping federal cuts targeting diversity, equity, and inclusion initiatives, Latino health leaders have launched the National Hispanic Health Research Institute — the first Latino-led community research hub designed to close glaring gaps in health data. The institute’s creation follows the cancellation of more than 600 NIH health disparities projects under President Donald Trump’s administration. NIH scientists criticized the policy, warning it “undermines the NIH mission, wastes public resources and harms the health of Americans and people across the globe.” Latino communities, already underrepresented in federally funded studies, are expected to be hit especially hard by the loss of research dollars. “Right now, we have both an opportunity and a responsibility to ensure that every family historically left out of the data is finally seen and counted,” said Ken Barela, the institute’s CEO. “When we’re missing from the research, our communities are erased, and when we’re erased, we’re left behind.” The new center plans to create a public health database that includes Latino, Afro-Latino, Native American, and rural populations. Its initial research will focus on maternal mortality, chronic disease, and youth health — areas where disparities are particularly severe. Dr. Andy Beltrán, the institute’s chief medical officer, emphasized that the mission goes beyond numbers. “The NHHRI serves not just as an engine for research, but as a guardian of equity,” he said. “By reimagining health research through the lived experiences of Hispanic families, we are laying the foundation for a healthier, more equitable America.” See: “Latino health leaders launch new institute to combat federal diversity cuts” (August 29, 2025)

Black Infant Deaths Surge in Mississippi
Mississippi has declared a public health emergency as infant mortality rates soar to levels not seen in over a decade. The crisis is hitting Black families hardest. In 2024, the state recorded 9.7 infant deaths per 1,000 live births—nearly double the national average. But for Black infants, the rate was a staggering 15.2, almost three times the national figure. “Too many Mississippi families are losing their babies before their first birthday,” said Dr. Dan Edney, the state’s top health officer. “We cannot and will not accept these numbers as our reality.”Since 2014, more than 3,500 infants in Mississippi have died before turning one. The spike in deaths is driven largely by newborns under 28 days old, according to March of Dimes CEO Cindy Rahman. She cited prematurity, birth defects, and maternal complications as key contributors. The disparity is stark: while Black infant deaths rose nearly 24% from 2023 to 2024, deaths among white infants declined. Experts link these outcomes to limited access to quality maternal care, especially in maternity care deserts—areas where prenatal services are scarce or nonexistent. Over half of Mississippi’s counties fall into this category. Medicaid plays a critical role, covering 53% of births in the state. Rahman warned that any cuts to Medicaid would worsen the crisis. “Mississippi has the knowledge, the resources, and the resilience to change this story,” Edney said. “It will take all of us.” See: “Mississippi’s Infant Mortality Crisis Raises Alarms” (August 25, 2025)

DACA Immigrants Face Rising Barriers to Health Care
Young immigrants protected under the Deferred Action for Childhood Arrivals (DACA) program continue to face severe health inequities, according to a new national report authored by researchers at the University of California, San Diego, in partnership with United We Dream, the National Immigration Law Center, and the Center for American Progress. The 2024 survey of more than 400 DACA recipients revealed that 19 percent were uninsured—over twice the national average for adults. Among those with coverage, 87 percent relied on employer-sponsored insurance, far higher than the general population, highlighting how access is tied closely to employment. More than 90 percent of respondents said that losing DACA would make it harder to keep themselves and their families healthy. Immigration status and cost concerns combined to worsen outcomes. One-third of recipients reported that stress over deportation harmed their physical or mental health. Sixteen percent said their conditions worsened because they skipped needed care. Nearly half avoided medical or dental treatments because of cost, and 16 percent rationed prescriptions. About 30 percent reported going into debt to cover medical expenses. The authors noted that policy changes have added to the instability. A Biden administration rule briefly allowed DACA recipients to enroll in Affordable Care Act plans, but a late 2024 court injunction blocked enrollment in 19 states. A new federal rule now ends that access nationwide, eliminating ACA subsidies and barring Medicaid and Medicare eligibility. The report concludes that these exclusions deepen health inequities for immigrant youth who grew up in the U.S. but remain locked out of its safety net. See: “DACA Recipients’ Access to Health Care: 2025 Report” (August 21, 2025)
Chronic Burden of Stress Worsens Breast Cancer Survival for Black Women
A new study from the University of Virginia reveals that allostatic load—the cumulative “wear and tear” the body experiences from chronic stress—plays a critical role in breast cancer outcomes and may help explain racial and geographic disparities in survival. Allostatic load is measured through biomarkers that track how stress disrupts multiple systems, including cardiovascular, metabolic, kidney, and immune function. When these systems are strained over time, the body becomes less able to recover, leaving individuals more vulnerable to disease. Researchers followed more than 3,000 women with stage I to III breast cancer. Black women had the highest average allostatic load scores, especially those living in rural areas. Rural Black women also faced the greatest mortality risk: each unit increase in their allostatic load score was linked to more than triple the risk of death compared to urban White women. Overall, patients with higher scores had significantly worse survival outcomes. Even after adjusting for age, socioeconomic status, tumor stage, and treatment factors, a high allostatic load was associated with a 27 percent greater risk of death. The study highlights how structural inequities—such as racism, poverty, and geographic isolation—directly influence biology. By embedding chronic stress into the body, these inequities accelerate health decline and worsen cancer survival. The authors stress that interventions addressing stress and its biological effects could be as vital as improving access to care in reducing disparities. See: “Allostatic Load and Racial and Rural Disparities in Breast Cancer Survival” (August 21, 2025)

Black Teens Least Likely to Receive Depression Care
A new study reveals troubling disparities in mental health treatment among U.S. adolescents, with Black teens significantly less likely to receive care for depression. Researchers found that fewer than half of adolescents diagnosed with a major depressive episode (MDE) in 2022 received any form of treatment, and only 39% saw a specialist. Using data from nearly 12,000 teens in the National Survey on Drug Use and Health, the study showed that 19.2% met the criteria for MDE. Among those, just 25% received prescription medication, and 30.5% accessed school-based services. But the gaps were even wider for marginalized groups. Black adolescents had the lowest odds of receiving any mental health treatment compared to their non-Hispanic white peers, with an adjusted odds ratio of 0.36. Rural teens also faced barriers, with significantly lower odds of accessing specialist care than those in urban areas. In contrast, female adolescents were more likely than males to receive treatment. “Addressing the disparities in mental health treatment revealed by this study is crucial for ensuring a more inclusive and equitable mental health support system,” the authors emphasized. The findings highlight the urgent need for targeted interventions to reach underserved youth, especially Black teens and those in rural communities. Without early recognition and care, adolescent depression can lead to long-term educational, health, and social consequences. See: “Few depressed teens getting treatment, study finds” (August 20, 2025)

Racial and Ethnic Minority Communities Face Higher Risk of Early Dementia
Young-onset dementia (YOD), which strikes before age 65, is disproportionately affecting racial and ethnic minority communities in the U.S., according to a new study of Medicare beneficiaries. Researchers found that Black, Hispanic, and American Indian and Alaska Native adults had significantly higher rates of YOD compared to White and Asian adults. Among 2.2 million Medicare beneficiaries aged 45 to 64, 3.25% had YOD. Black adults had the highest age-standardized prevalence at 3.76%, followed by White (3.23%), Asian (3.02%), Hispanic (2.73%), and American Indian and Alaska Native (2.69%) individuals. Notably, the proportion of YOD among all dementia cases was more than twice as high in Black, Hispanic, and American Indian and Alaska Native adults compared to White and Asian adults. The study also revealed that these groups carried a heavier burden of comorbidities linked to YOD. Black adults had the highest rates of hypertension and cardiovascular disease, while American Indian and Alaska Native adults had the highest prevalence of diabetes, alcohol use disorder, and traumatic brain injury. Traumatic brain injury was the strongest predictor of YOD across all groups, with American Indian and Alaska Native adults facing nearly 10 times the odds. Researchers emphasized the need for early screening and better care coordination, especially for younger adults in minoritized communities. “Improved early detection may help address the needs of Medicare beneficiaries with YOD,” they concluded. See: “Race and Ethnicity and Comorbidities Among Medicare Beneficiaries With Young-Onset Dementia” (August 20, 2025)

Fertility treatment and successful outcomes remain deeply unequal
Infertility affects millions of women in the U.S., but access to treatment and successful outcomes remain deeply unequal. A new study reveals that while 12% of women aged 20 to 44 report infertility, only 39% receive treatment—and just 10% achieve a live birth through fertility care. The disparities are stark. Among women with infertility, live birth rates were highest for Asian (17%) and White (13%) women, but plummeted for Hispanic (4%) and Black women (3%). The study found that higher education and private insurance significantly increased the likelihood of accessing treatment and having a successful outcome. “Black, Hispanic, and socioeconomically disadvantaged women face the greatest barriers to successful outcomes,” the authors wrote. These barriers include limited availability of services, inadequate insurance coverage, and restrictive legislation. Even though infertility awareness was relatively high (70%), the drop-off in treatment access and live births highlights systemic inequities. Using a cascade of care framework, researchers analyzed data from national surveys, birth certificates, and global infertility estimates. The findings show that fewer than half of women with infertility seek treatment, and only one in ten achieve a live birth. As more restrictive fertility laws emerge, the authors warn that these disparities may worsen. They urge health systems and policymakers to prioritize equitable access to fertility care, calling it “critical” for addressing the needs of underserved communities. See: “The Fertility Cascade: Infertility Prevalence, Access to Treatment and Successful Live Birth” (August 20, 2025)

Black men living in socioeconomically disadvantaged neighborhoods face higher odds of advanced prostate cancer
A new study reveals that men living in socioeconomically disadvantaged neighborhoods face significantly higher odds of being diagnosed with advanced prostate cancer, with Non-Hispanic Black men bearing a disproportionate burden of this disparity. Researchers from multiple institutions analyzed data from over 78,000 men diagnosed with prostate cancer in Michigan between 2004 and 2022. They used the Area Deprivation Index (ADI), which measures neighborhood socioeconomic status, to examine how poverty impacts cancer outcomes. The findings show a stark reality: patients living in the most disadvantaged areas were far more likely to present with aggressive disease. For every 10-point increase on the deprivation scale, a man’s odds of having metastatic prostate cancer at diagnosis increased by 4%. Non-Hispanic Black men, who represented 17% of the study population, were disproportionately concentrated in the most deprived neighborhoods—40.1% compared to just 5.4% in the least deprived areas. These men faced 1.52 times higher odds of metastatic disease compared to Non-Hispanic White men. “Our study underscores the silent barrier that socioeconomic deprivation poses to cancer early diagnosis,” the researchers noted in their conclusion. The disparities were evident across multiple measures of disease severity, including higher PSA levels, more advanced clinical stage, and higher-grade tumors. The research echoes growing concerns about how social determinants of health create unequal disease burdens and calls for “tailored interventions to bridge this gap” in prostate cancer care. See: “Socioeconomic disparities in Prostate Cancer Presentation: The impact of ADI on Prostate Cancer Stage at diagnosis” (August 19, 2025)

Gun Violence Devastates Black Communities, Profits Soar
In Bogalusa, Louisiana, gun violence has become a public health crisis, disproportionately impacting Black residents and leaving families shattered. Nineteen-year-old Tajdryn Forbes was shot and killed just weeks before he planned to leave the town. His death is one of many in a community where the violent crime rate is nearly twice the national average. Firearms are now the leading cause of death for children in the U.S., with young Black males suffering the highest toll. In 2023, more Black boys and men aged 15 to 24 were killed by guns than by the next 15 leading causes of death combined. “It has all the markers of an epidemic,” said Boston University’s Jonathan Jay. “Gun violence does not get the attention it deserves. It is underrecognized because it disproportionately impacts Black and brown people.” Despite the crisis, federal efforts to curb gun violence have been rolled back. The Trump administration repealed Biden-era policies aimed at regulating gun dealers and cut $820 million in grants for violence prevention. Surgeon General Vivek Murthy’s advisory declaring gun violence a public health emergency was removed within weeks of Trump’s inauguration. Meanwhile, the firearm industry thrives. With nearly 78,000 licensed gun dealers and record profits, political donations from gun manufacturers continue to influence policy. “People look at the demographic risk for firearm homicide and say, ‘Not my people, not my problem,’” said UC-Davis professor Garen Wintemute. See: “Guns, Race, and Profit: The Pain of America’s Other Epidemic” (August 19, 2025)
Fentanyl Crisis Hits Older Black Men Hardest
Synthetic opioids like fentanyl are driving overdose deaths among older Black men at alarming rates, yet few programs directly address their needs. In Minnesota, Black men aged 55 to 74 make up just about 1 percent of the population in Hennepin and Ramsey counties but accounted for more than 6 percent of overdose deaths between 2020 and 2024. Statewide, Black residents represent 7.5 percent of the population yet more than 19 percent of overdose deaths. Even as overall overdose deaths fell last year, this group continued to face some of the highest fatality rates. In Ramsey County, their death rate was nearly 16 times the national average. Public health discussions often focus on young people or the broader opioid crisis, leaving older Black men overlooked. A Minnesota legislative report on drug overdoses last year failed to mention older adults at all. One addiction doctor noted that opioid use disorder is often stereotyped as a “young man’s disease,” making it harder to detect in older populations. Community advocates say social inequities—housing instability, lack of insurance, and the legacy of incarceration—have compounded the crisis. “All of those things made a hell of a cocktail,” said Ivan Nelson, an addiction counselor who co-founded African American Survivor Services. His group recently launched programs tailored to older Black adults, emphasizing harm reduction and peer support. Without targeted interventions, advocates warn, this hidden generation will continue to face disproportionate risks. “Nobody’s looking at this hidden generation of folks that are dying in droves,” Nelson said. See: “Overdose deaths disproportionately impact older Black men” (August 18, 2025)

Black Mothers Face Worsening Mortality Gap After Pandemic
Maternal deaths among Black women in the United States surged during the COVID-19 pandemic and have not returned to pre-pandemic levels, even as mortality rates for White women declined, according to new national data. Between 2018 and mid-2024, more than 3.6 million Black women and 17 million White women gave birth. The pregnancy-related mortality ratio was 68 deaths per 100,000 live births for Black women, compared with 26.3 for White women. Similarly, maternal mortality stood at 46.5 for Black women, more than double the 17.6 recorded for White women. During the pandemic, deaths rose sharply for both groups, but Black women experienced the steepest increase. Their pregnancy-related mortality jumped by 29.4 per 100,000, compared with 11.8 among White women. Even after the public health crisis eased, disparities remained. Post-pandemic, Black women still faced nearly 10 additional deaths per 100,000 births compared with pre-pandemic rates, while outcomes for White women returned close to baseline. The result was a widening racial gap. Researchers point to systemic inequities—unequal access to prenatal and postpartum care, inconsistent insurance coverage, and racially biased medical practices—as drivers of the divide. These barriers often intersect with higher rates of hypertension, diabetes, and obesity in Black communities, conditions that compound pregnancy risks. The authors warn that the U.S. maternal mortality crisis now reflects not just a pandemic spike but an entrenched pattern of disparity. Placed in a global context, the findings are stark. While most high-income nations report maternal mortality rates of 10 or fewer per 100,000 live births, the rate for Black women in the United States remained above 50 in 2023. See: “Racial Disparities in Maternal Mortality Before, During, and After the COVID-19 Pandemic in the United States: A Difference-in-Difference Analysis” (August 18, 2025)

Health Disparities Drain Wealth in Black Communities
Poor health is costing Black Americans not only their lives but also their financial futures. Research highlighted in Rolling Out shows how chronic illnesses disproportionately affecting African Americans strip away billions in potential wealth, creating an underrecognized driver of economic inequality. Cardiovascular disease affects 60% of Black adults, a rate far above national averages. The toll is stark: Black Americans die from heart disease at rates 54% higher than whites, cutting off decades of earnings and preventing families from building generational wealth. Diabetes adds another layer of burden, with more than 12% of African Americans living with the disease compared with 7.4% of non-Hispanic whites. The costs are not limited to doctor bills—these conditions reduce energy, increase sick days, and force early retirements, depleting retirement savings meant to grow across generations. The ripple effects extend well beyond the patient. Families often see children struggle academically when parents are ill or acting as caregivers. Adult children may forgo promotions or leave jobs altogether to care for sick relatives. This cycle of diminished earning power locks entire families into economic vulnerability. The report stresses that preventive care, nutrition, and mental health support should be viewed as wealth-building strategies. Regular screenings, healthier diets, and community wellness programs could reduce costly chronic illnesses while preserving long-term earning power. As the piece concludes, investing in health is not simply a personal matter—it is a financial strategy essential to creating generational wealth in Black communities. See: “How poor health costs Black Americans billions in wealth” (August 15, 2025)

White patients visiting emergency rooms more likely to receive narcotic prescriptions than other racial groups
A new national study finds that racial and ethnic disparities in how patients are prescribed pain medication in U.S. emergency departments have not improved despite major shifts in pain management during the opioid crisis. Using data from more than 35,000 emergency visits for acute injuries, researchers compared prescribing patterns for White, Black, Hispanic, and other patients. They found that non-Hispanic White patients were consistently more likely to receive narcotic prescriptions than Black, Hispanic, and other racial groups, regardless of the time period studied. During the first wave of the opioid epidemic in the early 2000s, opioid prescribing in emergency departments rose sharply. By the second wave, efforts to curb opioid use led to more prescriptions for nonsteroidal anti-inflammatory drugs (NSAIDs) and other non-opioid medications. Yet the racial gap in prescribing did not change. White patients continued to receive opioids at higher rates, while Black and Hispanic patients were more likely to leave with non-opioid prescriptions or no medication at all. The findings echo decades of research showing that minority patients are more likely to be undertreated for pain. Prior studies have documented that Black and Hispanic patients receive fewer or lower doses of opioids for conditions ranging from kidney stones to fractures, compared to White patients. The persistence of these disparities, even as national prescribing practices evolved, highlights how bias and systemic inequities remain embedded in emergency care. See: “Racial Differences in Pain Medication Prescribed for Injury during Emergency Department Visits” (August 14, 2025)

Physician notes about Black patients more likely to question patient’s sincerity or competence
Clinicians are more likely to express doubt in the medical records of Black patients than White patients, according to a new study published in PLOS One. Researchers analyzed over 13 million electronic health records from a large health system and found that notes about non-Hispanic Black patients were significantly more likely to contain language questioning the patient’s sincerity or competence. Terms like “claims,” “insists,” or “poor historian” were flagged by artificial intelligence tools as indicators of doubt. While fewer than 1% of all notes contained such language, Black patients faced disproportionately higher odds of being described in ways that undermined their credibility. Compared to White patients, notes about Black patients were 29% more likely to contain credibility-undermining language and 50% more likely to question their competence. The study’s authors say this pattern may contribute to ongoing racial disparities in healthcare. “For years, many patients – particularly Black patients – have felt their concerns were dismissed by health professionals,” they wrote. They argue that biased documentation can stigmatize patients and affect the quality of care they receive. The researchers call for medical training that addresses unconscious bias and for AI tools used in clinical documentation to be programmed to avoid biased language. They believe their findings represent “the tip of an iceberg” and hope to raise awareness of credibility bias in healthcare. See: “Clinicians more likely to express doubt in medical records of Black patients” (August 13, 2025)

Health Disparities Research Defunded Amid Political Shift
Hundreds of federally funded research projects aimed at understanding and reducing health disparities have been abruptly canceled under the Trump administration’s second term, sparking alarm among scientists and public health advocates. The National Institutes of Health terminated at least 616 projects focused on closing health gaps between racial and socioeconomic groups. Nearly half of the $913 million in canceled awards had been earmarked for disparities research, including studies on maternal mortality, chronic disease, and access to care in underserved communities.Many researchers say their work was cut not for lack of merit, but because it included terms like “race,” “gender,” or “equity.” Dr. Kemi Doll, a cancer specialist, said the message was clear: “We do not value health equity.” One study, canceled and later reinstated, aimed to train doulas to support low-income mothers postpartum. Another, still defunded, sought to understand why Black women face higher risks of adverse birth outcomes by tracking biological aging. “It’s like they erased the problem,” said Dr. Jaime Slaughter-Acey, who is now seeking donations to complete the work. Critics argue that such research benefits all Americans. Programs originally designed for Black mothers, like sending blood pressure cuffs home after delivery, improved outcomes across racial groups. While the administration claims to support “all vulnerable populations,” many fear that eliminating targeted research will widen existing health gaps. “Disparity programs ask the question: Who are we missing, and why?” said Dr. Georges Benjamin. See: “Trump Administration Scraps Research Into Health Disparities” (August 13, 2025)

Black Mothers Face Rising Health Risks, Report Warns
Black women in the United States are dying during pregnancy and childbirth at alarming rates—two to four times higher than White, Hispanic, or Asian women. A new analysis from the McKinsey Institute for Economic Mobility and the McKinsey Health Institute reports that maternal mortality among Black women reached 50 deaths per 100,000 live births in 2023, and could nearly double by 2040 if current trends persist. Beyond mortality, Black women face disproportionate rates of serious conditions such as preeclampsia, gestational diabetes, and postpartum depression. These health challenges may not always be fatal, but they take a heavy toll. The report estimates that in 2025 alone, Black women giving birth will lose 350,000 healthy life years to disability and illness tied to maternal health. The disparities extend to infants. Black babies are more than twice as likely as their White, Hispanic, and Asian peers to die before their first birthday. Complications like preterm birth, low birth weight, and limited access to prenatal care are driving factors. Closing this gap could save 35,000 Black infants by 2040. The report also highlights broader costs. Maternal-health inequities not only devastate families but weaken the economy. Addressing the crisis could restore healthy years of life, save billions in healthcare spending, and add $24.4 billion to U.S. GDP through improved workforce participation. Underlying these disparities are structural drivers, including racism in healthcare, chronic disease burdens, and higher allostatic load—a biological marker of stress that shortens life and raises risks of hypertension, diabetes, and heart disease. See: “Closing the Black maternal-health gap: Healthier lives, stronger economies” (August 13, 2025)
Asian men least likely to receive prostate MRI for accurate diagnosis and treatment of prostate cancer
A recent meta-analysis has revealed troubling disparities in the use of prostate MRI among racial minority groups, with Black and Hispanic men receiving significantly less diagnostic imaging than their white counterparts. The study, published in Current Problems in Diagnostic Radiology, analyzed data from over 94,000 patients and found that Caucasian men were three times more likely to undergo prostate MRI than Black men. The gap was even wider for other groups. Only 19% of Black men received prostate MRI, compared to 66% of white patients. Hispanic men saw even lower rates at just 7%, and Asian men at 4%. These disparities extended to transrectal ultrasound (TRUS) use, with Black men again showing lower utilization. “Racial disparities in diagnostic imaging, particularly the use of multiparametric MRI (mpMRI) for prostate cancer, are associated with poor outcomes for Black patients,” wrote Ashkan Bahrami, MD, and colleagues. They noted that socioeconomic, geographic, and insurance-related factors accounted for more than 81% of the difference in mpMRI use. The authors emphasized that income and insurance coverage play a major role in access to advanced imaging. “Patients with a broader variety of insurance coverage and better incomes are more likely to seek advanced diagnostics imaging,” they stated. To reduce these disparities, the researchers advocate for policies that promote MRI-based protocols. They argue that mpMRI improves diagnostic precision and reduces unnecessary biopsies, especially for patients who lack comprehensive care. See: “Prostate MRI is significantly underutilized in racial minority groups” (August 12, 2025)

Cancer Patients’ Social Risks Often Go Undocumented
A new study reveals that social determinants of health (SDOH)—such as housing instability, isolation, and economic hardship—are rarely documented in the medical records of cancer patients, despite their known impact on outcomes. Using data from over 50,000 adults with cancer, researchers found that less than 2% had any SDOH-related Z codes in their claims, even though those with Z codes had significantly higher rates of comorbidities and metastatic disease. Z codes are diagnostic codes meant to capture individual-level social challenges. Yet 54% of oncologists surveyed had never heard of them. Only 19% had used them, and many cited lack of reimbursement and unclear clinical guidance as barriers. “Physicians are more likely to document Z codes if they’re tied to payer reimbursement,” the study noted. The most common Z codes included “problems related to living alone,” “occupational exposure to dust,” and “psychosocial circumstances.” These codes were more prevalent among women and patients in states with high out-of-pocket medical costs. Despite endorsements from CMS and the American Hospital Association, Z codes remain underutilized, limiting efforts to address disparities in cancer care. Researchers stress that better documentation is essential to understanding how social risks affect treatment and survival. Without it, public health initiatives and predictive models lack the data needed to support vulnerable populations. The study calls for increased provider awareness, financial incentives, and integration of SDOH into routine care. See: “Documentation of individual-level social determinants of health among adults diagnosed with cancer in the United States” (August 12, 2025)

Parkinson’s Research Excludes Many Blacks, Hispanics and Asians
Parkinson’s disease affects people of all racial and ethnic backgrounds, yet clinical trials and research continue to exclude many of them. According to 2023 NIH data, only 4% of Parkinson’s trial participants identified as Black, 3% as Asian, and 4% as Hispanic or Latinx—numbers far below their representation in the U.S. population. This lack of inclusion has real consequences for diagnosis, treatment, and access to care. Black Americans are more likely to be diagnosed at later stages, missing chances for early intervention. Latinx patients are less likely to see specialists trained in movement disorders. These disparities are not biological—they stem from systemic barriers in health care and research. Richard Huckabee, a young Black man, spent nearly nine years being misdiagnosed before finally learning he had Parkinson’s. His symptoms were dismissed, misattributed, and worsened by inappropriate medications. “There is no excuse,” he said, “just because I… do not fit the typical PD profile of an ‘old white male.’” The NIH’s Strategic Plan for Diversity, Equity, Inclusion, and Accessibility offers hope, but enforcement is weak. Researchers can still receive full funding without including diverse participants or reporting who was studied. To close the gap, experts call for tying funding to accountability, engaging communities with culturally relevant outreach, and investing in proven programs like Dance for PD® in multiple languages. Without sustained funding and inclusive practices, Parkinson’s research will continue to leave behind those who need it most. See: “Closing the diversity gap in Parkinson’s research” (August 12, 2025)

Redlined neighborhoods still more likely to lack rapid emergency medical service
A new nationwide study reveals that communities historically marked as “hazardous” on 1930s redlining maps are still suffering the consequences—this time in the form of delayed emergency medical services. These delays can be deadly, especially for patients experiencing trauma, stroke, cardiac arrest, or septic shock. Researchers found that residents in Grade D neighborhoods are 1.5 times more likely to lack rapid EMS access compared to those in Grade A areas. These same neighborhoods have fewer non-Hispanic white residents and more non-Hispanic Black residents, along with lower median incomes and higher population density. “Our findings reveal a novel and significant disparity,” said Dr. Dustin Duncan of Columbia University, “that adds to the growing body of literature on how redlining still impacts health outcomes today.” The consequences are serious. The National Fire Protection Association recommends EMS response within 9 minutes for general emergencies and 5 minutes for life-threatening ones. Failing to meet these benchmarks increases mortality risk, especially in underserved communities. The study calls for urgent reforms, including redistributing EMS units using geostatistical models, redesigning deployment protocols, and incorporating community input. Transparency and equity must guide future planning to ensure that historically marginalized neighborhoods receive the life-saving care they deserve . This research underscores how structural racism continues to shape access to healthcare, decades after discriminatory housing policies were enacted. See: “Historically Redlined Areas Face Disparities in Emergency Medical Access and Serious Consequences for Patients” (August 12, 2025)

Metabolic syndrome risks vary across Asian American communities
A national analysis of 2011–2016 NHANES data finds wide differences in metabolic syndrome (MetS) across Asian American subpopulations, challenging one-size-fits-all assumptions. MetS—a cluster of conditions that heighten risks for cardiovascular disease and type 2 diabetes—varied significantly by ethnicity and sex even within the same body mass index (BMI) ranges. Among women with BMI below 23, Filipinas had a 31.70% MetS prevalence compared with 14.45% among Chinese women. Among men with BMI 23–27.4, Asian Indian men showed 50.80% prevalence versus 22.66% in Vietnamese men. Gender patterns were notable. Across groups with BMI under 27.5, women generally had higher MetS prevalence than men; at BMI ≥27.5, rates were similar, with men slightly higher except in the Korean subgroup. Predicted probabilities underscored these gaps: at BMI 20, Asian Indian and Filipino men had higher MetS risks than Chinese and Vietnamese men, and Filipina women exceeded Vietnamese women; these disparities persisted at BMI 22, and Asian Indian men remained highest at BMI 24. In multivariable models, BMI and age were consistently linked to higher odds of MetS across all five ethnic groups. Two lifestyle factors showed subgroup-specific signals: current smoking was marginally associated with higher MetS among Filipino Americans, while high physical activity was marginally associated with lower MetS among Korean Americans; alcohol consumption was not significant. The authors emphasize that aggregated reporting masks critical intra-group differences and that disaggregated data are essential to inform targeted screening and prevention—particularly for higher-risk groups such as Filipino women and Asian Indian men. See: “Distinct metabolic syndrome profiles across Asian American subpopulations” (August 11, 2025)

Racial Gaps in Dental Care Widen Serious Oral Health Inequities
A recent study reveals that racial disparities in dental care affordability are contributing to serious oral health inequities in the United States. Among non-Hispanic Black adults, 21.03% reported being unable to afford needed dental care—nearly triple the rate of those at higher income levels. Mexican American and other Hispanic adults followed closely at 20.12%, underscoring the disproportionate burden faced by communities of color. These affordability barriers translate into worse health outcomes. Adults who couldn’t afford care were more than three times as likely to have untreated tooth decay and over four times more likely to suffer root caries. They also had higher DMFT scores—indicating more decayed and missing teeth—and fewer filled teeth, suggesting limited access to restorative treatment. The study highlights income as a major factor, with 31.03% of adults living below the federal poverty level unable to afford dental care. But without breaking out prevalence or treatment rates by race or ethnicity, the report misses a critical opportunity to fully expose the scope of racial disparities. This lack of detailed data makes it harder to design targeted interventions and track progress toward equity. Researchers call for expanding subsidized dental programs, increasing access in underserved areas, and promoting preventive care. But to truly address these disparities, future studies must include race-specific treatment data to ensure that solutions meet the needs of those most affected. See: “Dental care costs linked to major health disparities across age groups” (August 9, 2025)
Black Americans Face Higher Lupus Burden
A new national study reveals that systemic lupus erythematosus (SLE) disproportionately affects non-Hispanic Black adults in the United States. Using data from 2017 to 2021, researchers found that Black adults had more than twice the odds of having SLE compared to non-Hispanic Whites. Hispanic adults also showed elevated odds, though the difference was less pronounced. The study examined how social determinants of health (SDOH)—including income, insurance, psychological distress, and neighborhood conditions—correlate with SLE prevalence. Adults with Medicaid had significantly higher odds of SLE than those with private insurance. Those experiencing psychological distress or living in the Northeast also faced increased risk. Importantly, the report found that individuals with very high SDOH burden—defined as having eight or more unfavorable social factors—had more than triple the prevalence of SLE compared to those with low burden. Yet despite these findings, the report does not break out treatment rates or disease severity by race or ethnicity. This omission limits understanding of how systemic barriers affect disease management and outcomes in minority communities. “Non-Hispanic Black adults had higher odds of SLE,” the authors note, emphasizing that race, poverty, and insurance status are key drivers. Without detailed racial and ethnic breakdowns of treatment access and outcomes, policymakers and providers lack the data needed to address disparities effectively. See: “Association between social determinants of health and systemic lupus erythematosus: a nationally representative analysis of 2017–2021 data” (August 8, 2025)

Latino men are more than four times as likely to be diagnosed with HIV compared to their White counterparts
Latino men in the United States remain disproportionately affected by HIV/AIDS, with complex social and cultural factors driving higher risk. According to a new clinical trial, Latino men are more than four times as likely to be diagnosed with HIV compared to their White counterparts, and they accounted for nearly one-third of new HIV cases in 2022. Researchers tested HoMBRES de Familia, a culturally tailored program aimed at reducing the intertwined challenges of substance abuse, intimate partner violence, and HIV/AIDS—known as the SAVA syndemic. Conducted among 122 Latino fathers in Miami-Dade County, the study found the intervention significantly improved HIV knowledge and prevention self-efficacy. Six months after completing video-based sessions, participants in the intervention group answered 81% of HIV knowledge questions correctly, compared with 69% in the control group. The intervention also lowered risky sexual behaviors. Men in the intervention arm reported fewer instances of unprotected sex and multiple partners than those who only received a diabetes-prevention session. “By increasing self-efficacy and providing culturally sensitive content, these interactive video interventions can significantly reduce health disparities among Latino men,” the researchers reported. Alcohol use, however, presented a challenge. Both groups showed an increase in drinking quantity over the six-month period, a trend the authors linked to pandemic-related stress and anxiety. While binge drinking did not rise significantly, the overall uptick in consumption underscores the ongoing impact of social stressors on Latino health. The study concludes that culturally adapted, remote interventions can play a vital role in HIV prevention efforts, especially in minority communities facing barriers to healthcare access. See: “A randomized clinical trial testing the effectiveness of an adapted online HIV/AIDS prevention intervention among Latino men” (August 7, 2025)

Limited access to information technology linked to worse health outcomes among Black residents
Improving access to digital tools like broadband internet and smartphones could significantly reduce healthcare disparities for African Americans, according to researchers at UC Santa Barbara. Sharon Tettegah and Ebenezer Larnyo of the Center for Black Studies Research say that health technology—such as telehealth and health-related social media—can enhance care quality and access while reducing inequities. Larnyo, lead author of a study published in Frontiers in Public Health, emphasized that “higher socioeconomic status individuals are more likely to have technology access, and when they do have access, they experience fewer healthcare disparities.” The study analyzed data from 815 African Americans and found that limited access to technology correlates with worse health outcomes. The researchers point to systemic racism and economic inequality as root causes. Tettegah highlighted the case of tennis star Venus Williams, who suffered from undiagnosed uterine fibroids for years. “They were dismissing her,” she said, noting that many African American women face similar neglect in clinical settings. The study found that broadband internet and affordable smartphones are foundational to equitable care. But access alone isn’t enough. “We need culturally tailored telehealth, simple-to-use mental health apps, and health-related social media platforms,” Larnyo said. Tettegah added, “We need to build a narrative that highlights that with advocacy and information because often you don’t know that you don’t know.” See: “Better technology access reduces healthcare gaps for African Americans” (August 6, 2025)

Redlined Neighborhoods Wait Longer for Emergency Medical Help
Residents of historically redlined neighborhoods face slower emergency medical service (EMS) response times, a disparity that could cost lives. A new study published in JAMA Network Open found that more than 2.2 million people across 236 U.S. cities lack rapid EMS access—defined as a response time of five minutes or less. The study mapped EMS station locations and compared them to 1930s Home Owners’ Loan Corporation maps, which graded neighborhoods from A (“most desirable”) to D (“hazardous”). Grade D areas, often majority-Black and Hispanic, were deemed financially risky and denied mortgage loans. Today, those same areas are more likely to be underserved by EMS. Researchers found that roughly 7% of residents in D-graded neighborhoods lacked rapid EMS access, compared to about 4% in A-graded areas. The disparity was most severe in the Great Lakes region, where residents in redlined areas were nearly three times more likely to lack timely EMS care. The study also revealed fewer EMS stations in urban communities of color, contributing to longer wait times. “Delays in emergency care are associated with higher mortality rates,” the authors noted, especially during the critical “golden hour” following traumatic injury. The findings add to growing evidence that structural racism continues to shape health outcomes. Better tracking and accountability of EMS response times in marginalized communities could help close the gap. See: “Historically redlined communities have slower EMS response times” (August 5, 2025)
Breast Screening Criteria Miss Black Women
A new study reveals that Pennsylvania’s insurance criteria for supplemental breast cancer screening may unintentionally disadvantage Black women. The law covers women with extremely dense breasts or heterogeneously dense breasts plus a high lifetime risk of breast cancer. But these criteria rely on models and assessments that underestimate risk in Black women. Researchers analyzed over 68,000 mammograms and found that only 2.1% of Black women had extremely dense breasts, compared to 5.8% of White women. Just 0.7% of Black women had a lifetime breast cancer risk over 20%, versus 6.4% of White women. As a result, Black women were far less likely to qualify for supplemental screening—only 1.6% met the criteria, compared to 8.4% of White women.The consequences are serious. Among women who later developed cancer after a negative mammogram, none of the Black women would have been eligible for supplemental screening, while 29% of White women would have. “Our results suggest that expanding supplemental screening eligibility to all women with heterogeneously or extremely dense breasts would identify more false negatives,” the authors wrote. However, broadening access would dramatically increase the number of MRIs, raising costs and straining resources. The study calls for better risk models that include race, BMI, and other factors to more accurately identify women at risk—especially Black women, who face higher rates of aggressive cancers and breast cancer mortality. See: “Racial Differences in Screening Eligibility by Breast Density” (August 5, 2025)

Redlined Neighborhoods Wait Longer than White Neighborhoods for Emergency Help
A new study reveals that residents of historically redlined neighborhoods face significantly slower emergency medical service (EMS) response times—an inequity with life-threatening consequences. Published in JAMA Network Open, the research mapped EMS centers across 236 U.S. cities and compared them to 1930s Home Owners’ Loan Corporation maps, which labeled majority-Black areas as “hazardous” for investment. The findings are stark: roughly 7% of residents in D-graded neighborhoods lack rapid EMS access, defined as a response time of five minutes or less. In contrast, only 4% of residents in A-graded, predominantly white neighborhoods face the same delay. In the Great Lakes region, the odds of lacking rapid EMS access were nearly three times higher for residents in redlined areas. These delays are not just inconvenient—they’re deadly. For traumatic injuries, the first 60 minutes, known as the “golden hour,” are critical. Longer EMS response times have been linked to higher mortality rates, especially in low-income ZIP codes. The study adds to mounting evidence that structural racism continues to shape health outcomes. Redlined communities still struggle with lower life expectancy, higher pollution exposure, and now, slower emergency care. Researchers call for better tracking and accountability to address these disparities. See: “Historically redlined communities have slower EMS response times, study shows” (August 5, 2025)

Women living in deprived areas 20% more likely to develop gestational diabetes
Living in a resource-poor neighborhood may significantly increase a woman’s risk of developing gestational diabetes mellitus (GDM), according to new research from the University of Arizona. The study examined over 480,000 births across 15 counties and found that women in deprived areas were 20% more likely to develop GDM—a condition with long-term health consequences for both mother and child. Researchers used the Neighborhood Deprivation Index, which factors in housing quality, violence, education, access to healthy food, and poverty. “Where you live can influence your health,” said Melissa Furlong, Ph.D., senior author of the study. “It can impact stress, access to quality food, the ability to interact with the outdoors and exercise—all factors that can affect health.” The findings were especially concerning for Native American communities, where GDM incidence reached nearly 18%, more than double the general population rate. Women in poorer neighborhoods were also more likely to be younger, less educated, overweight, and reliant on public insurance. Furlong emphasized the need for policy changes, including eliminating food deserts and expanding access to quality housing and prenatal care. “We know there are racial disparities in GDM,” she said, “and we wanted to go beyond that and more fully gauge the importance of social determinants of health at a neighborhood level.” See: “Resource-poor neighborhood conditions may increase gestational diabetes risk” (August 5, 2025)

Social Advantage, Not Job Complexity, May Protect Against Cognitive Decline
A new study sheds light on why Black Americans face higher risks of cognitive decline and dementia than their White peers—and it’s not about how mentally demanding their jobs were. Instead, it’s about the social advantages that come with higher-status occupations. Researchers from the University of Michigan and other institutions analyzed data from over 500 older adults in the Michigan Cognitive Aging Project. They found that Black participants were significantly less likely to have held high-status jobs, and this occupational gap explained up to 7% of the racial disparities in memory and thinking skills. “Occupation may influence cognitive disparities primarily through socioeconomic, rather than cognitive stimulation, pathways,” the authors wrote. Contrary to the popular “use-it-or-lose-it” theory, the study found that the mental, social, and physical demands of a job—collectively known as occupational complexity—did not explain racial differences in cognitive performance. Even when jobs were mentally engaging, they didn’t offer the same protective benefits if they weren’t accompanied by higher income or wealth. The disparities were most pronounced among participants who were no longer working. For them, lower education, lower-status jobs, and lower income combined to create a cascade of disadvantage that harmed cognitive health. The researchers argue that addressing structural barriers to education and employment could help reduce these disparities. “Policies targeting workforce inequities may reduce racial disparities in dementia risk,” the study concludes, pointing to the need for systemic change rather than individual job choices. See: “Occupational position and complexity in relation to Black-White cognitive disparities” (August 4, 2025)

Hispanic men have most extensive vulnerability to brain injury from high blood pressure, diabetes, smoking
A new study examining brain health disparities among men reveals striking differences in how cardiovascular risk factors affect white matter damage across racial and ethnic groups. Researchers analyzed brain scans and health data from 1,378 men participating in the Health and Aging Brain Study-Health Disparities. The research found that Hispanic men showed the most extensive vulnerability to brain injury from conditions like high blood pressure, diabetes, and smoking. Every cardiovascular risk factor examined was linked to increased white matter hyperintensities—brain lesions that appear as bright spots on MRI scans and signal vascular damage that can lead to cognitive decline and Alzheimer’s disease. “Hispanic males exhibited the broadest vulnerability: hypertension, diabetes, and tobacco dependence each predicted higher WMH,” the researchers reported. Even small increases in blood pressure measurements significantly worsened brain damage in Hispanic men, an effect not seen in white or Black men. Black men showed a more selective pattern, with hypertension and diabetes linked to brain injury, while white men had the most limited associations, primarily with high blood pressure.The findings highlight concerning healthcare disparities, as the same cardiovascular conditions that put men at highest risk for brain damage often exclude them from Alzheimer’s treatment trials. “These individuals are doubly disadvantaged: they face a greater likelihood of cognitive decline and yet may be ruled out of disease-modifying therapies,” researchers noted. The study underscores the urgent need for targeted cardiovascular interventions to protect brain health in minority communities. See: “Racial and Ethnic Differences in Cardiometabolic Predictors of White Matter Hyperintensities Burden Amongst Males – The HABS-HD Study” (August 4, 2025)

Blacks and Hispanics in nursing homes less likely to have access to Alzheimer’s Disease special care units
Black and Hispanic residents in U.S. nursing homes are significantly less likely to have access to Alzheimer’s disease special care units (ASCUs), according to a new study published in JAMA Network Open. These specialized units, which improve outcomes for people with dementia, are available in only 13.6% of nursing homes nationwide. The study analyzed data from over 13,000 facilities and found that nursing homes with higher percentages of Black residents were up to 45% less likely to offer ASCUs. Facilities with more Hispanic residents also showed reduced access, though disparities were less responsive to policy changes. Researchers found that Medicaid reimbursement rates play a critical role. In states where Medicaid payments covered a greater share of care costs, racial disparities in ASCU availability narrowed—and in some cases, disappeared. In states with the most constrained Medicaid funding, nursing homes with high proportions of Black residents were 68% less likely to have ASCUs. That gap shrank to 45% in moderately funded states and was statistically insignificant in states with the most generous Medicaid payments. “Racial disparities in specialized dementia care may be mitigated and even eliminated by more generous Medicaid payments,” the authors concluded. However, disparities for Hispanic residents persisted regardless of funding levels, highlighting the need for more accurate data collection and targeted policy solutions. See: “Medicaid Payments and Racial and Ethnic Disparities in Alzheimer Disease Special Care Units” (August 4, 2025)

Depression and loneliness critical, yet often overlooked, contributors to hypertension in Black women
A new study reveals that depression and loneliness are critical, yet often overlooked, contributors to hypertension in Black women—deepening disparities in cardiovascular health. Researchers at George Washington University reviewed 23 studies spanning 15 years, focusing on Black women in the U.S. diagnosed with high blood pressure. Hypertension affects over half of Black women, compared to 39% of non-Hispanic white women. Yet only a quarter of those affected have their condition under control. The review found that Black women with hypertension face significantly higher risks of depression and report elevated levels of loneliness. These emotional burdens are not just side effects—they may directly raise blood pressure, especially in midlife and older women. Lead author Lashawn Hutto emphasized that standard depression screening tools often fail to capture how Black women express distress. “Standard tools miss too many women who are silently suffering,” she said. “We must adopt culturally responsive approaches that recognize how racism, loneliness, and emotional distress are deeply intertwined with physical health.” The study also highlighted systemic barriers: uninsured Black women are less likely to receive treatment for depression and more likely to encounter physicians who overlook psychosocial concerns. Researchers call for routine screening for depression and loneliness in chronic illness care, and for care teams to be trained in trauma-informed, culturally sensitive practices. See: “New Study Reveals Critical Links Between Depression, Loneliness, and Hypertension in Black Women” (August 4, 2025)

Black babies nearly three times more likely to be born prematurely than White babies in San Francisco
In San Francisco, Black babies are now nearly three times more likely to be born prematurely than white babies—a disparity that has reached its highest level since the state began tracking the data in 2007. While the city’s overall preterm birth rate is below the state average, the rate for Black infants has surged to 16%, compared to just 6% for white infants. This widening gap is not just statistical—it’s deeply personal. Teaja Watts gave birth to her daughter Kaori at just 25 weeks. “I just didn’t know if she was going to live or not,” she said. Kaori has spent over six months in the neonatal intensive care unit. Despite the crisis, San Francisco has failed to fully invest in maternal health programs designed to address these disparities. The city’s Black Infant Health Initiative has been chronically understaffed and has returned millions in unused state funds. From 2021 to 2024, the city underspent its maternal equity budget by $7.3 million. Programs like the Abundant Birth Project, which provided direct financial support to Black and Pacific Islander parents, showed promise. “It gave me the ability to provide for my kids,” said participant Sabrina Hall. But the project was halted amid legal challenges claiming racial discrimination. “We need to listen to this data,” said pediatrician Zea Malawa. “It’s screaming at us to do something.” See: “Black babies in SF are at greater risk of early birth than ever” (August 4, 2025)

Black Men With Prostate Cancer Less Likely to Receive Key Treatment Tests
Black men newly diagnosed with prostate cancer are significantly less likely than white men to receive confirmatory testing within the first year—a critical step in ensuring accurate diagnosis and appropriate treatment. A recent study published in JAMA Network Open found that Black men had a 6.1 percent lower rate of completing these tests, with an adjusted odds ratio of 0.75 compared to white men. Confirmatory testing helps determine whether active surveillance is appropriate or if more aggressive treatment is needed. Without it, patients may miss the opportunity for timely intervention or, conversely, undergo unnecessary procedures. The lack of testing raises concerns about the quality of care Black men receive and whether systemic barriers are influencing clinical decisions. The study also revealed that Black men were less likely to be overtreated than white men, particularly among those considered unhealthy. While overtreatment can lead to complications and reduced quality of life, the lower rate among Black men may reflect disparities in access rather than better care. “Our study highlights the importance of understanding the nuanced relationship between utilization and prostate cancer care quality when trying to improve care for underserved communities,” the authors wrote. These findings underscore the urgent need to address racial gaps in cancer care. Ensuring that Black men receive appropriate diagnostic follow-up is not just a matter of equity—it’s a matter of survival. See: “Racial Differences Seen in Prostate Cancer Care Quality” (August 4, 2025)

Puerto Ricans in U.S. more likely to die from asthma than their peers on the island
Puerto Ricans living in the United States die from asthma at higher rates than their counterparts on the island, and education plays a critical role in those disparities. A new study in The Journal of Allergy and Clinical Immunology: In Practice shows that Puerto Ricans with lower educational attainment face particularly steep risks, challenging long-held assumptions about Hispanic health advantages. Researchers found that Puerto Rican individuals in the U.S. with less than a high school degree had an asthma mortality rate of 38.86 per 100,000, compared with 22.37 per 100,000 among Puerto Ricans in Puerto Rico. Even with a high school diploma, mortality was far higher stateside—46.3 per 100,000 compared with 15.45 per 100,000 on the island. By contrast, non-Hispanic white individuals with the same education levels had mortality rates less than one-third as high. The findings undermine the so-called Hispanic Mortality Paradox, which has suggested that Hispanic immigrants often live longer than non-Hispanic whites despite socioeconomic disadvantages. “Education contributes to reducing [asthma mortality] but impacts inconsistently [Puerto Rican] populations, suggesting that other factors are at play,” said lead author Sylvette Nazario, MD, of the University of Puerto Rico Medical Sciences Campus. Socioeconomic context appeared to influence these outcomes. Puerto Ricans on the island had lower incomes, higher poverty rates, and greater dependence on public insurance, but higher educational achievement did not translate into the same health gains as it did for Puerto Ricans in the U.S. or for other groups. The study highlights how location, education, and community resources intersect to shape asthma-related mortality, placing Puerto Ricans alongside non-Hispanic Black individuals as the populations at highest risk. See: “Asthma mortality in Puerto Rican individuals differs by U.S. vs. Puerto Rico residence” (August 1, 2025)

Only half of Latino adults receive needed mental health treatment
In 2023, only 48% of Latino adults who needed mental health services received treatment. The consequences have been devastating. Between 2010 and 2020, suicide rates among Latino men rose nearly 36%, and among Latinas, by over 40%. “No one should suffer in silence,” Senators Alex Padilla said. “We need to break down the barriers that keep Latinos from getting the mental health care they need.” Ruben Gallego added, “This issue is personal to me. Too many Latinos, especially men, shy away from seeking help because they’re afraid of being judged.” Latino communities across the U.S. face persistent barriers to mental health care, and a new bill introduced by California and Arizona lawmakers aims to change that. The Mental Health for Latinos Act, unveiled by Senators Alex Padilla and Ruben Gallego, along with Representatives Andrea Salinas and Nanette Barragán, seeks to provide culturally and linguistically tailored mental health resources. The bill directs the Substance Abuse and Mental Health Services Administration to launch a public health strategy that meets diverse cultural and language needs, raises awareness of mental illness symptoms, and promotes evidence-based treatments. It also emphasizes community participation and the link between behavioral and physical health. Endorsed by major organizations including UnidosUS and the National Alliance on Mental Illness, the legislation reflects growing recognition that mental health care must be inclusive to be effective. See: “California Senators Introduce Mental Health for Latinos Act” (August 1, 2025)

Mistrust Blocks Black Participation in Clinical Trials
Medical mistrust continues to keep Black Americans out of clinical trials, with serious consequences for health outcomes. A recent study led by Dr. Shakira J. Grant explored how historical trauma and personal experiences shape attitudes toward medical research among Black patients with multiple myeloma. Through interviews with patients and caregivers, the study revealed that Black participants often carry a “deep, transgenerational knowledge” of medical mistreatment, including the infamous Tuskegee syphilis experiment. This legacy of unethical research, combined with ongoing disparities in healthcare access and outcomes, fosters a persistent mistrust. “These personal stories highlighted a pervasive mistrust that impacted their willingness to participate in clinical trials,” Dr. Grant said. The result is a lack of representation in studies that determine how treatments work—leaving Black patients at risk of receiving therapies that haven’t been adequately tested for their needs. Clinical trials depend on diverse participation to ensure safety and effectiveness across populations. Without it, gaps in medical knowledge grow, and disparities in treatment outcomes widen. Dr. Grant emphasized that building trust requires transparency, acknowledgment of past wrongs, and more Black healthcare providers. “Trust takes years to gain and a second to lose,” she said. The impact is not just academic—it’s deeply personal. Mistrust can mean fewer treatment options, poorer outcomes, and continued inequity. Healing this divide will take sustained effort from researchers, clinicians, and communities alike. See: “Medical Mistrust Keeps Black Americans Out of Clinical Trials” (July 31, 2025)

Black stroke patients receive fewer life-saving treatments than White patients even in the same certified hospitals
Despite a decade of progress in stroke care, Black patients continue to receive fewer life-saving treatments than White patients—even when treated at the same certified hospitals. A new study of over 2.1 million Medicare stroke admissions reveals that stroke center certification significantly boosted treatment rates for White patients, but not for Black patients. When hospitals became certified as primary stroke centers, White patients saw a 31% increase in thrombolytic therapy. That number jumped to nearly 68% at more advanced centers. Black patients, however, saw no statistically significant change in access to thrombolytics, even at the same facilities. Mechanical thrombectomy rates also rose sharply for White patients—by over 500%—after hospitals gained advanced certification. Black patients experienced a modest 137% increase, despite starting from a lower baseline. “These within-hospital differences…serve as sobering evidence that significant barriers persist,” the authors wrote. The disparities weren’t explained by age, comorbidities, or hospital type. Instead, researchers pointed to systemic issues: Black patients are less likely to use emergency services, more likely to arrive late to the ER, and face longer wait times. They’re also more likely to refuse treatment. Even as stroke centers expanded and patient volumes grew, the racial gap in treatment widened. The study concludes that broader insurance coverage alone isn’t enough. Targeted education and structural reforms are needed to ensure equitable stroke care. See: “Stroke Center Certification and Within-Hospital Racial Disparities in Treatment” (July 30, 2025)

Teen Suicide Rates Drop, But Racial Data Missing
New federal data show a decline in teen suicide rates, with serious suicidal thoughts among 12- to 17-year-olds falling from nearly 13% in 2021 to 10% in 2024. Suicide attempts also dropped slightly, from 3.6% to 2.7%. Experts say this is a hopeful sign, possibly linked to more teens opening up about their struggles and accessing treatment tailored to suicide prevention. But, “this report does not break out prevalence or treatment rates by race or ethnicity,” said Hannah Wesolowski of the National Alliance for Mental Illness. That omission is raising concern among mental health advocates because without that data, she warned, it’s harder to track whether progress is reaching all communities equally. Wesolowski pointed out that suicide rates among Black youth have been rising rapidly in recent years. “Are we making progress on that?” she asked. Without racial and ethnic data, there’s no way to know. A spokesperson from the Department of Health said demographic data will be released in a forthcoming report. But for now, the lack of transparency leaves a gap in understanding how different communities are faring—and whether interventions are equitably distributed. Despite the encouraging trends, suicide remains one of the leading causes of death among teens. Advocates say the need for more comprehensive data and targeted support remains urgent. See: “New federal data show a decline in teen suicide” (July 30, 2025)
Black Americans continue to face stark disparities across the entire colorectal cancer care continuum
Black Americans continue to face stark disparities across the entire colorectal cancer care continuum—from screening and diagnosis to treatment and survival. Despite overall declines in colorectal cancer incidence and mortality, Black patients remain disproportionately affected, with higher rates of late-stage diagnosis and lower survival outcomes. The gap begins with screening. Black adults are less likely to receive timely colonoscopies, and even when screened, they are more likely to experience delays in follow-up care. These delays contribute to more advanced disease at diagnosis, which in turn worsens prognosis. Treatment disparities are equally troubling. Black patients are less likely to receive guideline-concordant care, including surgery and chemotherapy. They also face longer wait times and are more likely to be treated at lower-resourced hospitals. The cumulative effect is a survival rate that lags behind that of white patients. Structural racism and social determinants of health play a central role. Factors such as insurance status, income, and neighborhood segregation influence access to care and quality of treatment. The article emphasizes that “addressing disparities in colorectal cancer requires a multifaceted approach,” including policy reform, community engagement, and culturally tailored interventions. Researchers call for more inclusive clinical trials and better data collection to understand the full scope of these inequities. Without targeted efforts, the racial gap in colorectal cancer outcomes is likely to persist. See: “Black–White disparities across the colorectal cancer care continuum in the USA” (July 29, 2025)
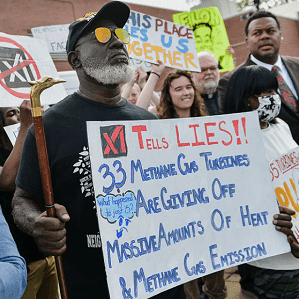
Artificial Intelligence Expansion Pollutes Black Communities
Artificial intelligence may promise convenience, but its environmental cost is falling hardest on Black neighborhoods. In a powerful reflection, Rev. Dr. Heber Brown III reveals how AI infrastructure is deepening environmental racism in places like Boxtown, a historic Black community in South Memphis. Just three miles from Boxtown, Elon Musk’s xAI supercomputer facility is releasing smog and harmful chemicals through gas turbines. “Residents are saying that they can barely breathe,” Brown writes. The facility joins more than 17 industrial sites in the area, compounding pollution and health risks. Boxtown residents face increased rates of asthma, heart disease, and a cancer risk more than four times the national average. Brown, who once embraced AI for ministry work, changed course after witnessing its impact. “Artificial Intelligence, as currently engineered, is an environmental disaster,” he says. Each AI task consumes massive energy, pumping pollution into the air, water, and soil. The decision to build in Boxtown, he argues, is no accident—it’s part of a legacy of environmental neglect targeting Black communities. As founder of the Black Church Food Security Network, Brown emphasizes that food justice and environmental stewardship must go hand-in-hand. “We cannot compromise our ethics in the name of convenience,” he writes. Until AI industries are guided by racial and environmental justice, he refuses to promote them. “Protecting the profits of the richest white men in the world will never be worth more than a single human life,” Brown concludes. See: “Artificial Intelligence Furthers Environmental Racism in Black America” (July 28, 2025)

Why Black Families Face Barriers to Swimming
Drowning is the leading cause of death among children ages 1 to 4. This danger is magnified for Black families, as the fatal drowning rate for African American children is three times higher than for white children. The disparities in water safety are a result of systemic issues, historical racism, and inherited fear. Historically, Black Americans were kept out of public pools through violence and segregation during the 1920s through the 1940s. When the Civil Rights Movement pressured for integration, some municipalities chose to close pools rather than open them to everyone, making swimming lessons and access a privilege for those who could afford private pools. These historical barriers have created a lasting impact. A USA Swimming study found that if a parent does not know how to swim, there is only a 13% chance their child will learn how. This inherited fear and lack of role models in the water have been passed down through generations. Finding available classes remains difficult, as many facilities shut down during the pandemic, and the remaining lessons are often expensive and in high demand. Despite the challenges, organizations like Swim 4 Life, Black People Will Swim, and Outdoor Afro are working to provide solutions for underserved communities. See: “Why Black Families Face Barriers to Swimming” (July 28, 2025)

Older Hispanic adults who lose all their natural teeth may face faster cognitive decline
Older Hispanic adults who lose all their natural teeth may face a steeper decline in cognitive function than their peers who retain their teeth. A new study analyzing data from over 23,000 participants found that edentulism—complete tooth loss—was linked to faster cognitive aging, especially among Hispanic individuals. While Hispanic and Black adults began with lower cognitive scores than white participants, their decline was generally slower. But for Hispanics without teeth, that protective trend disappeared. Their cognitive scores dropped about 0.03 points faster per year than those with teeth—a small but potentially significant difference over time. Researchers suggest several reasons for this link. Tooth loss can impair chewing, reducing blood flow to brain regions tied to memory. It may also reflect chronic gum disease, which fuels inflammation—a known contributor to brain aging. Poor nutrition from avoiding certain foods could further worsen cognitive health. Though Hispanic participants had the lowest rates of edentulism, they also had the lowest levels of education and household wealth. These social disadvantages may compound the effects of tooth loss. Interestingly, Black participants did not show the same accelerated decline, possibly due to stronger social support or lifelong exposure to poor oral health. Regular dental visits were associated with better cognitive scores, highlighting the value of preventive care. The study underscores how disparities in oral health can ripple into brain health, and why access to dental care should be part of broader efforts to reduce health inequities. See: “Tooth loss linked to faster cognitive decline in Hispanic older adults” (July 26, 2025)

Biological differences may explain why Black women experience more aggressive and lethal breast cancers
Research from the University of Notre Dame reveals biological differences that may explain why Black women experience more aggressive breast cancers and higher mortality rates compared to white women. While breast cancer incidence is highest among white women, Black women are more likely to develop early-onset or aggressive subtypes like triple-negative breast cancer. The disparity becomes stark among younger women. Young Black women under 50 have double the mortality rate of young white women with breast cancer, according to the study published in iScience.Scientists discovered that a specific population of cells called PZP cells may contribute to this health inequality. These cells are naturally and significantly higher in healthy breast tissues of women of African ancestry compared to women of European ancestry. The research showed that PZP cells send signals that prompt other breast cells to become invasive and detach from their original location. “The disparity in breast cancer mortality rates, particularly among women of African descent, is multifaceted,” said Crislyn D’Souza-Schorey, the study’s corresponding author and Morris Pollard Professor of Biological Sciences at Notre Dame. She noted that while socioeconomic factors and delayed diagnosis contribute, “substantial emerging evidence suggests that biological and genetic differences between racial groups can also play a role.” The findings emphasize the need for inclusive cancer research and treatment approaches that account for biological variations across racial groups to improve outcomes for all women. See: “Women of African ancestry may be biologically predisposed to early onset or aggressive breast cancers” (July 24, 2025)

Cancer Deaths linked to Obesity surge for Black Americans and Native Americans
Obesity-related cancer deaths have tripled in the United States since 1999, with Black Americans and other marginalized groups bearing the brunt of the increase. A study presented at ENDO 2025 revealed that mortality rates from obesity-associated cancers rose from 3.7 to 13.5 deaths per million over two decades. The impact is not evenly distributed. Women, older adults, Native Americans, Black Americans, and residents of rural areas saw the most significant increases. “Obesity is a significant risk factor for multiple cancers, contributing to significant mortality,” said lead researcher Faizan Ahmed, MD. He emphasized the urgent need for early screening and better access to care in high-risk communities. Obesity affects more than 40% of U.S. adults and is linked to 13 types of cancer, including breast, colon, uterine, and pancreatic. These cancers account for 40% of all diagnoses annually. Yet, the burden falls disproportionately on communities already facing systemic barriers to healthcare. Regional disparities also emerged. The Midwest had the highest rate of obesity-related cancer deaths, while the Northeast had the lowest. States like Vermont, Minnesota, and Oklahoma topped the list, contrasting with lower rates in Utah, Alabama, and Virginia. The findings highlight a pressing public health challenge: addressing obesity and cancer through targeted interventions that prioritize equity. Without action, the toll on underserved communities will continue to rise. See: “Obesity-Linked Cancer Deaths Tripled Since 1999” (July 23, 2025)

Persistent lack of physician diversity is quietly fueling disparities in health care access and outcomes
A persistent lack of physician diversity is quietly fueling disparities in health care access and outcomes across communities of color. According to analysis from KFF, Hispanic, Black, American Indian and Alaska Native (AIAN), and Native Hawaiian and Pacific Islander (NHPI) individuals remain starkly underrepresented among physicians, despite growing demand for racially concordant care. The mismatch is most striking for Hispanic people. Though they represent 20% of the U.S. population, they make up only 7% of the physician workforce. In states like New Mexico, where Hispanics constitute nearly half the population, they account for just 17% of physicians—a gap of 31 percentage points. Similarly, Black Americans are 12% of the population but just 6% of physicians nationwide, with particularly wide disparities in the Southeast and D.C. These gaps have real consequences. Data show that racial concordance between patients and doctors is linked to increased preventive care, better treatment adherence, and even reduced mortality. Yet most Hispanic, Black, Asian, and AIAN adults report that fewer than half of their health care visits were with a provider who shared their racial or ethnic background. Policy changes may be compounding the problem. The Supreme Court’s 2023 decision to end race-conscious college admissions has already led to a drop in medical school matriculation rates among underrepresented groups. As federal diversity initiatives face rollbacks, the physician pipeline appears increasingly vulnerable—threatening progress toward equitable care. See: “Physician Workforce Diversity by Race and Ethnicity” (Jul 22, 2025)

Latinos Face Elevated Risk of Nerve Damage in their hands and feet
Latinos in the United States may be at significantly higher risk for peripheral neuropathy—a condition marked by pain, tingling, and numbness in the hands and feet—than their white counterparts, according to new research published in Neurology. The study, which surveyed over 8,000 adults, found that 13% had peripheral neuropathy, with Latinos showing a 32% increased risk even after adjusting for health, lifestyle, and social factors. Study author Evan Lee Reynolds, PhD, of Michigan State University, noted that “race and ethnicity are social constructs without a biological basis and may be proxy… for hard-to-measure risk factors.” Despite controlling for known contributors like blood sugar, cholesterol, physical activity, and income, Latino participants still showed elevated odds of nerve damage. Social vulnerabilities appeared to amplify the risk. Being uninsured increased the likelihood of neuropathy by 56%, while food insecurity raised it by 48%. Reynolds emphasized that “unknown social risk factors exist for this population,” urging future studies to dig deeper into what might be driving these disparities. The findings suggest that Latino communities may be facing hidden burdens that standard health metrics fail to capture. With peripheral neuropathy affecting not just sensation but digestion and urination, the stakes are high for early detection and equitable care. See: “Latinos May Be at Increased Risk for Nerve Damage” (July 18, 2025)

Older White Men most at-risk for suicide, especially by firearms
While youth suicide has drawn national attention, older white men remain the most at-risk group—yet their crisis is often overlooked. CDC data show that men aged 75 and older have the highest suicide rates in the country, with 38.2 deaths per 100,000 among those 75–84 and 55.7 among those over 85. Among these, white men are disproportionately affected. Silvia Canetto, a psychology professor at Colorado State University, notes that suicide is especially high among men of European descent. These men often don’t face severe social or health challenges, but they do share traits like emotional stoicism, narrow self-identity, and reluctance to express vulnerability. “These indignities of aging happen to everyone,” she said, “but suicide is not equally common.” Firearms play a deadly role. Older white men are far more likely to die by gun suicide than women, with rates 51 times higher among men over 85. Rosie Bauder explains that firearms are lethal in 95 out of 100 suicide attempts, leaving little room for intervention. Social isolation compounds the risk. Igor Galynker describes how men often lose meaning and connection after retirement. “Men spend their life achieving and neglect social connections,” he said. Daniel Coleman adds that men are taught to suppress emotions, making it harder to seek help. Experts urge targeted public health campaigns that reframe therapy as strength and promote social connection. As Paul Nestadt puts it, “It’s about finding a message that resonates.” See: “Suicide rates rising in older men, CDC data reveal” (July 17, 2025)

Black Mothers Face Higher Risk, Less Support for Postpartum Depression
Postpartum depression is rising across the U.S., but for Black women, the crisis is deepening. Since 2010, the rate of postpartum depression among Black mothers has nearly tripled, reaching almost 25% by 2021. Yet, they remain 46% less likely to be screened and far less likely to receive treatment compared to white women. Kay Matthews knows this disparity firsthand. After the stillbirth of her daughter in 2013, she was released from the hospital with no support, no follow-up, and no acknowledgment of her trauma. “I got no pamphlets, no follow-up information, nothing,” she said. Her grief spiraled into postpartum depression, but no one diagnosed her. “Simply because they looked at my birth outcome,” she said.Matthews later founded the Shades of Blue Project, a nonprofit supporting women with postpartum depression. Her experience, she says, “made me realize how prevalent racism is within the healthcare system.” Dr. Joy Baker, an obstetrician in rural Georgia, also learned the hard way. One of her patients, overwhelmed by untreated postpartum depression, died by suicide. “It just wasn’t on my radar,” Baker admitted. Mental health conditions like depression and anxiety now account for 23% of maternal deaths, according to the CDC. With Medicaid covering nearly half of all births in states like Georgia, upcoming federal cuts could devastate access to care. “We will go backwards,” Baker warned. Matthews added, “The impact for what’s to come is going to be astronomical.” See: “Black Women Often Need More Help Fighting Postpartum Depression” (July 17, 2025)

Extremely Severe Obesity Surges in Black Youth
Extremely severe obesity in children has surged by 253% over the past 15 years, with the steepest rise among non-Hispanic Black adolescents aged 16 to 18. A new study analyzing data from over 25,800 participants in the National Health and Nutrition Examination Survey reveals that obesity is not only increasing but becoming more severe—prompting researchers to propose new classifications beyond the current three-tier system. Children in the newly defined class 4 and 5 obesity categories—those with a BMI 160% to over 180% of the 95th percentile—face alarming health risks. Every child in these categories showed signs of insulin resistance, compared to 81% in lower obesity classes and just 27% among children with healthy weights. These children also had significantly higher rates of diabetes, metabolic disease, and liver complications. The burden is not just clinical. Families face mounting costs and emotional strain, while the public health system grapples with the long-term consequences. “The findings of this study… provide robust evidence supporting extremely severe obesity specifically as a public health emergency,” the authors warn, calling for early prevention, targeted education, and mobilization of resources.Without urgent intervention, the trajectory of obesity-related illness in minority youth threatens to deepen existing health disparities and overwhelm care systems already stretched thin. See: “Extremely severe obesity is on the rise in kids—along with a barrage of health problems” (July 17, 2025)

COVID Hit Black and Hispanic Kids Harder
Black and Hispanic children faced sharply higher hospitalization rates for COVID-19 during the first three years of the pandemic, a multi-state analysis published in JAMA Network Open reveals. Based on more than 13,500 cases across 12 states, the study found that hospitalization rates were over twice as high for Black children (2.15 times) and Hispanic children (2.06 times) compared to Asian or Pacific Islander peers. These disparities deepened when children were admitted to intensive care. ICU admission was 1.88 times higher for Black children and 2.13 times higher for Hispanic children. Most hospitalizations occurred in children under age 4, and even within that age group, Black and Hispanic kids were disproportionately affected. Though hospitalization rates declined after 2022, researchers noted the racial gaps persisted. “Hospitalization rates among Black and Hispanic children remained consistently higher compared with Asian or Pacific Islander children for each period,” they wrote. Nearly all children hospitalized—regardless of race—had not received the recommended COVID vaccine. The authors suggest that underlying conditions such as asthma and chronic illness, particularly among Black children, may contribute to elevated risk. They emphasized the urgent need to increase vaccination uptake and early treatment access to reduce inequities. This report adds to a growing body of research underscoring how racial and ethnic disparities continue to shape children’s vulnerability in public health crises. See: “Analysis shows higher COVID hospitalization rates for Black, Hispanic kids” (July 16, 2025)
Black youth exposed to violence and danger in childhood face accelerated aging and increased cardiac risk as adults
Black youth exposed to violence and danger in childhood face more than immediate trauma—they carry the burden into adulthood through accelerated aging and increased cardiac risk. A new study tracking 449 Black Americans from age 10 to 29 found that early exposure to danger predicted elevated alcohol consumption later in life, even among those who didn’t drink heavily as teens. This delayed effect, called “incubation,” links childhood adversity to adult health problems through immune system changes. Researchers found that exposure to danger altered DNA methylation in FKBP5, a gene tied to inflammation. That change was associated with higher alcohol use at age 29, which in turn led to faster biological aging and increased cardiac risk. The study’s lead author, Steven R.H. Beach, explains that these effects are independent of early substance use. “We found a significant incubation pathway from childhood danger to elevated alcohol consumption and then to health outcomes,” he writes. The impact was stronger for Black men in terms of alcohol use, but Black women showed greater vulnerability to its health consequences. These findings underscore the long-term toll of structural racism and community violence. Black children are more likely than white children to witness beatings, shootings, and other traumatic events. The study suggests that these experiences don’t just shape behavior—they rewire biology. Efforts to reduce health disparities must begin early, with safer environments and stronger support systems. Without intervention, the damage of childhood danger may silently unfold for decades. See: “Childhood exposure to danger increases Black youths’ alcohol consumption, accelerated aging, and cardiac risk as young adults: A test of the incubation hypothesis” (July 16, 2025)

Black and Hispanic children faced sharply higher hospitalization rates for COVID-19
Black and Hispanic children faced sharply higher hospitalization rates for COVID-19 during the first three years of the pandemic, a multi-state analysis published in JAMA Network Open reveals. Based on more than 13,500 cases across 12 states, the study found that hospitalization rates were over twice as high for Black children (2.15 times) and Hispanic children (2.06 times) compared to Asian or Pacific Islander peers. These disparities deepened when children were admitted to intensive care. ICU admission was 1.88 times higher for Black children and 2.13 times higher for Hispanic children. Most hospitalizations occurred in children under age 4, and even within that age group, Black and Hispanic kids were disproportionately affected. Though hospitalization rates declined after 2022, researchers noted the racial gaps persisted. “Hospitalization rates among Black and Hispanic children remained consistently higher compared with Asian or Pacific Islander children for each period,” they wrote. Nearly all children hospitalized—regardless of race—had not received the recommended COVID vaccine. The authors suggest that underlying conditions such as asthma and chronic illness, particularly among Black children, may contribute to elevated risk. They emphasized the urgent need to increase vaccination uptake and early treatment access to reduce inequities. This report adds to a growing body of research underscoring how racial and ethnic disparities continue to shape children’s vulnerability in public health crises. See: “Analysis shows higher COVID hospitalization rates for Black, Hispanic kids” (July 16, 2025)

Obesity-Linked Cancer Deaths Surge in Minorities
Cancer deaths tied to obesity have tripled in the U.S. over the past two decades, with sharp increases among Black Americans, Native Americans, older adults, and women. A study presented at ENDO 2025 analyzed more than 33,000 deaths from obesity-associated cancers between 1999 and 2020, revealing that age-adjusted mortality rates rose from 3.73 to 13.52 per million. Lead researcher Faizan Ahmed emphasized that “obesity is a significant risk factor for multiple cancers,” and called for targeted public health strategies, especially in underserved and rural areas. The Midwest had the highest regional death rates, while Vermont, Minnesota, and Oklahoma topped the state-level list. Obesity’s impact is not just statistical—it’s biological. Excess visceral fat triggers inflammation, which can damage the body and increase cancer risk. This inflammation stems from fat cells that lack oxygen, disrupting hormone regulation and fueling disease. Ahmed urged a shift from downstream management to upstream prevention. He proposed universal access to cancer screening, public campaigns that normalize obesity management, and policies promoting healthy food and physical activity. He also called for incentives to integrate weight management into routine care and investment in community-based models for underserved populations. With 40.3% of U.S. adults classified as obese, the stakes are high. The study’s findings underscore how obesity intersects with race, geography, and access to care—deepening health disparities and demanding urgent attention. See: “Obesity-Linked Cancer Death Rate Triples in U.S.” (July 16, 2025)

Women of Color, Especially Black Women, Face Delays in Endometrial Cancer Surgery
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black Patients More Likely to Make frequent Trips to Emergency Departments for Seizures
Emergency departments are seeing a troubling pattern: frequent visits for seizures among patients from low-income and minority communities. Emergency departments are not equipped to manage chronic conditions like epilepsy long-term. Instead, they treat acute episodes, which can be avoided with proper ongoing care. A study published in Epilepsia reveals that socioeconomic and racial disparities are driving this trend, with nearly 15% of over 200,000 patients returning to the ER more than once during the study period. Patients with Medicare, Medicaid, or no insurance were significantly more likely to have repeat emergency visits compared to those with private insurance. Black patients, in particular, had higher odds of frequent ER use than white patients. However, when Black patients had public insurance, the disparity was less pronounced. Those living in the lowest-income zip codes were also more likely to be frequent ER users. Frequent emergency visits are not a sign of good care. They often reflect a lack of access to consistent outpatient treatment and preventive services.The authors of the study stress that solving these disparities requires more than just medical intervention. “Eliminating deeply rooted factors such as poverty, health care costs, and systemic racism requires comprehensive, multisectoral approaches far beyond the scope of health care providers alone,” they write. Still, they urge clinicians to advocate for patients and push for policy changes that address these systemic issues. See: “Socioeconomic Disparities Contribute to Frequent ED Visits for Seizure” (July 14, 2025)
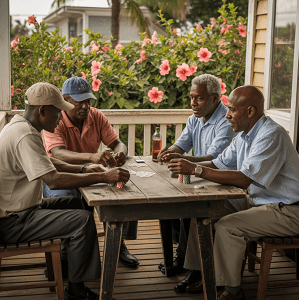
Nearly half of Black retirees leave workforce earlier than planned due to health issues or disabilities
Retirement is often seen as a reward for a lifetime of work, but for many Black Americans, it’s a phase marked by financial strain and health challenges. New research from the Employee Benefit Research Institute reveals that nearly half of Black retirees left the workforce earlier than planned due to health issues or disabilities—compared to just one-third of non-Black retirees. This disparity underscores how health inequities continue to shape lives long after employment ends. Poor health outcomes, often tied to environmental exposures, unsafe workplaces, and limited access to quality care, force early retirement. That means fewer years of earning, reduced Social Security benefits, and faster depletion of savings. The result is a retirement marked by financial stress and ongoing health management, rather than rest and security. The impact doesn’t stop there. Two-thirds of Black retirees report needing to return to work for financial reasons, compared to just over one-third of non-Black retirees. Many take lower-paying or part-time jobs, despite health limitations, just to stay afloat. Debt adds another layer of complexity. Among higher earners, nearly two-thirds of Black Americans say debt threatens their financial security, compared to less than half of their non-Black peers. These burdens reflect systemic barriers to wealth accumulation and compound the challenges of retirement. The report calls for systemic solutions—not just better financial planning. Without addressing the root causes of inequality in health, employment, and housing, retirement will remain out of reach for many. See: “Retirement exposes the fault lines in the American promise” (July 11, 2025)

Young adults from disadvantaged backgrounds may age faster at cellular level
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Critically ill Black patients in ICU less likely to have genetic diagnoses
A new study reveals that nearly one-quarter of critically ill adults admitted to intensive care units had genetic conditions linked to their symptoms—yet half of them were unaware of these diagnoses. This lack of awareness can mean missed opportunities for targeted treatment and better outcomes. But the most troubling finding is the racial disparity in who gets diagnosed. Black patients were significantly less likely than white patients to have their genetic conditions documented before or during their ICU stay. While 63% of white patients had known diagnoses, only 23% of Black patients did. This gap matters: patients with documented genetic conditions were more likely to survive their hospitalization. The study did not break down the prevalence or treatment rates of these conditions by race or ethnicity, a limitation that obscures the full scope of disparities. Without this data, it’s harder to understand how systemic barriers—like limited insurance, lack of racial diversity among doctors, and mistrust of the medical system—impact diagnosis and care. “Getting a genetic diagnosis often requires a series of steps,” said Monica Wojcik, a clinical geneticist. Black patients are more likely to fall through the cracks in this complex process. Latrice Landry, a computational geneticist, emphasized the need to raise awareness and simplify access to testing. “The solution is multipronged,” she said, “but it is attainable.” See: “Genetic testing of critically ill adults can yield surprises—and reveal disparities in treatment of Black patients” (10 July 2025)
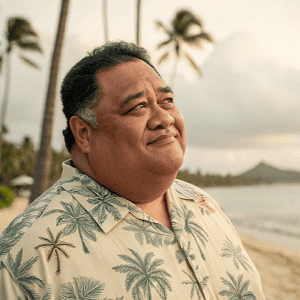
Steep increases in obesity rates for Native Hawaiian and other Pacific Islanders
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Heart risk tool accurately predicts cardiovascular events in diverse Asian and Hispanic populations
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black Veterans Wait Longest When Referred for Specialty Care
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Cancer Patients of Color Less Likely to Message Doctors
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black and Hispanic Adults Lag Behind Whites and Asians for Lung Cancer Screening
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Immigrants Fear Seeking Health Coverage Could Lead to Deportation
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black and Latino patients less likely to have received antiviral prescriptions to treat COVID-19
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Medicaid improved disparities in care and survival for patients with chronic liver disease
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black Patients Face More Epilepsy Emergency Room Visits
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black Americans with both diabetes and hypertension in midlife have higher risk of dementia
A new study from the University of Georgia reveals that poor heart health in midlife may significantly increase the risk of dementia for Black Americans. Researchers found that individuals diagnosed with both diabetes and hypertension had elevated levels of a dementia-related biomarker more than a decade later. “This matters,” said Rachael Weaver, the study’s lead author. “Chronic conditions like high blood pressure and diabetes, especially when combined together, might start damaging the brain earlier than we thought, especially for this group.” The study followed over 250 participants and found that having both conditions—not just one—led to a greater increase in the biomarker over an 11-year period. Black Americans already experience cognitive decline at higher rates and younger ages than White individuals, making these findings especially urgent. Karlo Lei, a co-author, emphasized that “taking steps early to control high blood pressure and diabetes may help protect African Americans from brain degeneration.” The researchers suggest that cardiovascular health should be prioritized as a key indicator of dementia risk. Socioeconomic factors also played a role. Nearly 20% of participants had less than a 12th-grade education, and many reported low incomes. Weaver noted, “Health inequities like the ones that we’re exploring are not inevitable. They are very systemic, and they’re potentially preventable.” The study calls for early intervention and public health education in at-risk communities to reduce the burden of neurodegenerative diseases. See: “Poor heart health increases risk of dementia for Black Americans” (July 4, 2025)

Black adolescents in high-risk urban areas more likely to be screened for depression than their peers
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Mexican American cancer patients face disparities in palliative care
New research presented at ASCO 2025 reveals troubling disparities in palliative cancer treatment among Hispanic patients in the United States, with certain national origins facing significantly reduced access to care. The study, led by Edward C. Dee, MD, and Shriya Garg, analyzed data from the National Cancer Database, focusing on patients with stage 4 breast, lung, and prostate cancer. “We wanted to see if there were disparities in Hispanic subgroups,” Garg explained, noting that previous studies often lump Hispanic patients into broad categories. Their analysis disaggregated the data by national origin, uncovering stark differences. Patients of Mexican descent showed consistent disparities in receiving palliative interventions across all three cancer types. Those of South or Central American and Cuban descent were less likely to receive palliative care for lung and breast cancer. Dominican patients had significantly reduced uptake of palliative care for breast cancer compared to White patients. The researchers emphasized that these disparities are not just statistical—they reflect deeper systemic issues. “It could be religion or language or cultural norms or preferences, end-of-life care preferences, cost, immigration status, or financial toxicity,” Garg said. These factors can shape how patients engage with care and whether they receive the support they need. To address these gaps, the team advocates for culturally sensitive approaches, greater involvement of families and communities in care decisions, and improved patient engagement. Tailoring interventions to specific populations could make palliative care more accessible and equitable. See: “ASCO 2025: Palliative Care Gaps in Hispanic Patients With Cancer” (July 2, 2025)

Overdose Deaths Decline, But Racial Gaps Widen
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black patients treated in for opioid overdoses less likely to receive referrals for addiction treatment
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black Women Face Sharp Rise in Endometrial Cancer Deaths
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Asian Adolescents Face Barriers in Asthma Diagnosis and Care
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.
Mosquito Control Gaps Leave Vulnerable Communities at Risk
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Stress and discrimination may account for quarter of greater dementia risk for Black older adults
A new study reveals that chronic stress and perceived discrimination may account for nearly a quarter of the racial disparity in dementia risk between Black and White older adults in the United States. Researchers analyzed data from over 5,600 participants in the nationally representative Health and Retirement Study and found that Black individuals had more than twice the risk of developing dementia compared to White individuals. While neither chronic stress nor discrimination directly mediated the relationship between race and dementia, both factors significantly interacted with race to elevate risk. Eliminating racial differences in either chronic stress or perceived discrimination could reduce the Black-White dementia disparity by approximately 24% and 25%, respectively. “These findings suggest that interventions should focus on Black individuals who experience high levels of stress and discrimination,” the authors wrote. The study used validated measures, including the Everyday Discrimination Scale, and accounted for variables such as education, income, and genetic risk factors. Prior research has shown that Black Americans report higher levels of discrimination and stress, which are linked to poorer cognitive outcomes and increased brain lesions associated with dementia. This study adds to growing evidence that social determinants of health—particularly those rooted in systemic racism—play a critical role in long-term cognitive health. The authors emphasized the need for targeted public health strategies to address these stressors and reduce the disproportionate burden of dementia in Black communities. See “Investigating the role of chronic stress and perceived discrimination in racial disparities in incident dementia among U.S. older adults” (July 1, 2025)

Segregated Neighborhoods Linked to Higher Lung Cancer Risk
A major new study has found that African American adults living in highly segregated neighborhoods face a significantly higher risk of developing lung cancer. The research, which followed over 71,000 participants across 12 southern U.S. states, revealed that reducing residential segregation could lower lung cancer incidence among African Americans—but not among non-Hispanic White individuals. The study used the isolation index to measure segregation and found that African American participants had a median index of 0.8, compared to 0.2 for White participants. Lowering this index in hypothetical scenarios led to fewer lung cancer cases. For example, reducing segregation to the least segregated quartile was associated with nearly 37 fewer cases per 10,000 people. Menthol cigarette use emerged as a major factor. Among African Americans, 52.5% primarily smoked menthols, compared to just 17.4% of White participants. Menthol smoking alone accounted for nearly 25% of the link between segregation and lung cancer. Air pollution, secondhand smoke at home, and lower education levels also played significant roles. Researchers concluded that 47% of the segregation-lung cancer link could be explained by these mediators. However, over half of the risk remained unexplained, pointing to deeper structural issues. “This study suggests the need for urgent policy addressing structural racism and its mediators that prevent lung cancer,” the authors wrote. See: “Residential Segregation and Lung Cancer Risk in African American Adults” (July 1, 2025)
Expanding lung cancer screening guidelines could help close racial disparities
A new study suggests that expanding lung cancer screening guidelines could help close persistent racial and gender disparities in healthcare. Researchers found that current U.S. Preventive Services Task Force (USPSTF) criteria—originally set in 2013—often exclude women and Black individuals who are still at risk for lung cancer. The USPSTF had already revised its guidelines once, lowering the age from 55 to 50 and reducing the smoking history requirement from 30 to 20 pack-years. But disparities remain. “Women and Black people, in particular, often did not qualify for lung cancer screening despite still being susceptible to the disease,” the study noted. By comparing several screening models, including those from the American Cancer Society and Potter criteria, researchers found that more inclusive guidelines significantly increased eligibility. Under the Potter criteria, 55% of women and 35% of Black individuals qualified for screening, compared to just 48% and 22% under USPSTF rules. Even though expanded criteria slightly reduced screening efficiency, they led to 28% more cancers being detected. “Our study suggests that relaxed smoking history requirements may provide better access… while maintaining diagnostic efficiency,” the researchers concluded. This shift could be a critical step toward health equity, ensuring that more people—especially those from historically underserved communities—are diagnosed earlier, when treatment is more effective. See: “Expanding preventive screening advice may boost health equity” (Jun 30, 2025)

Black Women Enter Menopause Earlier, Suffer Longer
Black women in the U.S. are entering menopause earlier, enduring more severe symptoms, and receiving less care than their white counterparts, according to a growing body of research. The disparities are not just biological—they’re systemic. The median age of natural menopause is 52.17 for Black women, nearly nine months earlier than for white women. But the difference goes beyond timing. Black women experience vasomotor symptoms like hot flashes and night sweats for an average of 10.1 years—compared to 6.5 years for white women. They are also twice as likely to undergo surgical menopause and 50% less likely to use hormone therapy beforehand. Despite the intensity of symptoms, many Black women don’t recognize them as signs of perimenopause. That’s partly because most healthcare providers aren’t trained to recognize them either. Only 31% of OB/GYN residency programs in the U.S. offer a menopause curriculum—and most are elective. The lack of culturally competent care compounds the problem. Black women are more likely to report depression, worse sleep, and more intense symptoms, yet their experiences are often undocumented in medical records. This leads to fewer referrals and prescriptions, even in systems designed to be equitable. Researchers point to the “weathering hypothesis”—the idea that chronic stress from racism accelerates health decline—as a key factor. Without intervention, these disparities could lead to higher risks of cardiovascular disease, osteoporosis, and mental health disorders. “Black Women Face Earlier Menopause Onset and Inadequate Care” (June 29, 2025)

Usual photo technologies poor at capturing skin conditions in people with darker skin tones
A new guide is challenging the status quo in dermatology by calling attention to how poorly traditional photography captures skin conditions in people with darker skin tones. The issue, experts say, is more than technical—it’s about equity, trust, and better care. “Traditional photographic technologies have typically been calibrated using lighter skin tones,” said Dr. Nada Elbuluk, co-author of the guide and director of the USC Skin of Color and Pigmentary Disorders Program. This has led to inaccurate depictions of dermatologic conditions in patients with skin of color, contributing to diagnostic gaps and underrepresentation in medical education. The guide, published in JAMA Dermatology, offers practical solutions: use of dark backgrounds, soft lighting, cross-polarization, and standardized distances. But it also emphasizes humanistic practices like informed consent and preserving patient dignity during photography. High-quality images, Elbuluk explained, can improve clinical monitoring and care, especially for pigmentary disorders. They also help diversify educational materials, which have long lacked accurate images of skin conditions in non-white patients. “This guide isn’t just about how to take better clinical photographs,” Elbuluk said. “It’s about health equity, patient trust, and clinical excellence.” The next step, she noted, is to develop standardized clinical guidelines and integrate these practices into dermatology training. As clinicians adopt more inclusive imaging techniques, they can help close the diagnostic gap and improve outcomes for underrepresented populations. See: “Best Practices for High-Quality Pictures in Patients With Skin of Color” (June 27, 2025)
Black Patients Face Higher Risks After weight-loss surgery
Black Americans undergoing weight-loss surgery are experiencing significantly more minor complications than their White counterparts, according to new research presented at the American Society for Metabolic and Bariatric Surgery’s annual meeting. The study, led by Dr. Safraz Hamid of Yale University, analyzed data from over 1.1 million patients who had either laparoscopic sleeve gastrectomy or Roux-en-Y gastric bypass between 2016 and 2023. Each year, Black patients showed higher rates of Clavien-Dindo category 1 complications, rising from 10.2 percent in 2016 to 15.0 percent in 2023, compared to 7.6 to 12.1 percent among White patients. While more severe complications (CD2 through CD5) did not show consistent racial differences, other indicators of post-surgical strain did. Readmission rates were consistently higher for Black patients, starting at 5.2 percent in 2016 and dropping to 3.7 percent in 2023, compared to 3.5 and 2.8 percent for White patients. Emergency department visits also rose for both groups, but remained significantly higher among Black patients—11.0 percent in 2023 versus 8.3 percent for White patients. Dr. Hamid expressed concern over the persistent disparities and the upward trend in minor complications. “We were surprised the minor complication rate increased year after year and that racial disparities persisted,” he said. “More work is needed to identify what’s causing the uptick and how it can be reversed.” See: “Minor Complications Up for Black Patients After Weight-Loss Surgery” (June 27, 2025)

Felt discrimination, childhood adversity linked to hypertension in Black communities
A new study from rural Alabama reveals how the weight of racial discrimination and early-life adversity may be contributing to high blood pressure among Black adults. Researchers found that both perceived racial discrimination and childhood adversity were significantly associated with self-reported hypertension in predominantly Black communities. The study, conducted in five rural Alabama towns, surveyed 184 adults using paper-and-pencil questionnaires. Ninety-two percent of participants identified as Black. Researchers measured perceived racial discrimination using a subscale of the African American Historical Trauma Questionnaire and assessed childhood adversity with the ACE Study Questionnaire. Older age and higher scores of perceived racial discrimination were both linked to increased odds of high blood pressure. Specifically, each increase in perceived discrimination was associated with a 15% rise in the likelihood of reporting hypertension. “Disproportionate exposure to psychosocial stressors, such as racial discrimination, and other forms of adversity across the life course contributes to higher rates of hypertension among Black Americans,” the authors wrote. They emphasized that rural populations are often underrepresented in health research, despite facing unique barriers to care. The findings underscore the need for trauma-informed, culturally tailored interventions to address health disparities in rural Black communities. The authors call for multilevel strategies that go beyond individual behavior change and address the structural roots of chronic disease. See: “Perceived Racial Discrimination, Childhood Adversity, and Self-Reported High Blood Pressure among adults in Rural Alabama” (June 27, 2025)

Black and Hispanic patients less likely to receive key medications for opioid use disorder
A new study published in JAMA Network Open found that Black patients were 17.1% less likely and Hispanic patients 16.2% less likely than white patients to receive buprenorphine or naltrexone within six months of a substance use-related health event. “We’ve seen rising overdoses and rising overdose deaths in racial and ethnic minoritized communities, particularly Black Americans,” said Dr. Utsha Khatri, lead author and assistant professor at the Icahn School of Medicine at Mount Sinai. She attributed much of the disparity to lack of access to effective medications. The study analyzed data from 176,000 health events across Medicaid, Medicare Advantage, and private insurers. It found that patients with government-backed insurance were more likely to receive treatment than those with commercial plans. However, the study did not include methadone, often considered the most effective treatment, due to its strict regulations. Tracie Gardner, founder of the National Black Harm Reduction Network, pointed to systemic issues: limited health services in communities of color, stigma around medication-assisted treatment, and incarceration policies that often deny access to care. “This medieval stuff is still infused in what we’re calling a 21st-century addiction treatment setting,” she said. Khatri emphasized the need for culturally sensitive care and expanded Medicaid access. “Not all communities are benefiting equally,” she warned, urging policymakers to protect and expand safety-net programs. See: “Black, Hispanic patients significantly less likely to receive key addiction medications, study finds” (June 26, 2025)
Black and Hispanic Teens with Diabetes Face Gaps in Use of glucose monitors
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Latino Neighborhoods in Los Angeles Face Deadlier Heat, Dirtier Air
Latino communities in Los Angeles are bearing the brunt of climate change and environmental neglect, according to new data from UCLA’s Latino Policy and Politics Institute. The Latino Climate and Health Dashboard reveals that Latino-majority neighborhoods experience 25 extreme heat days per year—more than triple the number in white-majority areas. “Extreme heat isn’t just uncomfortable, it’s deadly,” said Irene Burga of Green Latinos. These neighborhoods often lack tree cover, have older housing without modern cooling systems, and are home to workers in heat-exposed jobs. Tree canopy covers just 4% of land in Latino neighborhoods, compared to 9% in white areas. The dashboard, supported by the California Wellness Foundation, also shows higher exposure to air pollution and worse health outcomes, including asthma and emergency room visits. “Latino communities are on the front lines of climate change, yet they’ve often been left out of the data and decisions,” said UCLA professor Arturo Vargas Bustamante. The situation is worsened by recent immigration enforcement actions. “People are staying home,” said Mar Velez of the Latino Coalition for a Healthy California. “They’re scared of encountering ICE, then having health issues, heat strokes.” In a city where air conditioning isn’t required in rentals, fear and heat can be a deadly combination. Advocates hope the dashboard will empower communities and lawmakers to act. “Uncovering and really understanding the layers of impact,” Velez said, “is something I’m really looking forward to.” See: “The profound environmental health disparities between Latino and white neighborhoods in L.A.” (June 24, 2025)
Cancer Rates Reveal Gaps in HIV Care for Minorities
A new study reveals that Florida’s mosquito control system may be reinforcing public health disparities, with wealthier areas receiving better protection against mosquito-borne diseases like dengue, West Nile, and Zika.

Black infants 60% more likely than Whites to suffer brain injury from oxygen deprivation
A new study published in the Journal of Perinatology reveals stark racial disparities in the diagnosis, severity, and treatment of hypoxic-ischemic encephalopathy (HIE), a serious brain injury caused by oxygen deprivation at birth. Analyzing data from over 31 million births between 2010 and 2018, researchers found that African American newborns were 60% more likely to develop HIE than white infants and twice as likely to experience severe forms of the condition. The disparities didn’t stop at diagnosis. African American infants with HIE had significantly higher overall mortality rates, with an adjusted odds ratio of 2.14. However, when comparing only infants already diagnosed with HIE, mortality rates between Black and white babies were similar. The study also found that Native American infants were significantly less likely to receive hypothermia therapy, the standard treatment for HIE. Their odds of receiving this potentially life-saving intervention were less than half that of white infants. “Racial disparity exists in the prevalence, severity, and management of HIE,” the authors concluded. These findings underscore the urgent need for equitable access to neonatal care and interventions that can reduce long-term disability or death. The research highlights how systemic inequities in healthcare continue to affect the most vulnerable—newborns—at the very start of life. See: “Racial disparities and outcomes in neonatal hypoxic-ischemic encephalopathy” (June 21, 2025)

Sharp rise in fatal falls among older Americans, especially White seniors
A new CDC report reveals a sharp rise in fatal falls among older Americans, with white seniors disproportionately affected. From 2003 to 2023, death rates from unintentional falls surged more than 70% for adults aged 65 to 74, over 75% for those 75 to 84, and more than doubled for people 85 and older. In 2023 alone, more than 41,000 retirement-age Americans died from falls—about one in every 56 deaths in that age group. More than half of those deaths occurred among people 85 and older, and 87% of those were white. “Kind of a flip of the traditional disparity lens,” said Geoffrey Hoffman, PhD, MPH, a University of Michigan researcher, noting that older Black adults had the lowest fall-related death rate. The reasons behind this racial disparity remain unclear. Experts suggest that differences in how falls are reported and classified on death certificates may play a role. Geographic variation also stood out: Wisconsin had the highest fall-related death rate, more than five times that of Alabama, the lowest. Ice and wintry weather may contribute, but reporting practices and other unknown factors are likely involved. Falls can lead to serious injuries like head trauma or broken bones, which often trigger a cascade of health complications. Age-related changes in vision, hearing, and medication side effects are common contributors. As the population ages, understanding why white seniors are dying at higher rates from falls could help shape more effective prevention strategies. See: “Older Adults in the U.S. Are Increasingly Dying From Unintentional Falls” (June 19, 2025)
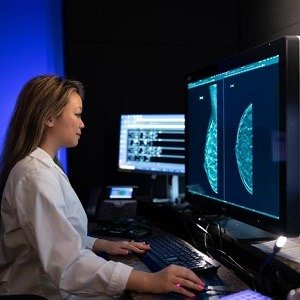
Dropping Mammogram Fees Boosts Access for Underserved Communities
Removing a modest $45 fee for 3D mammography led to a measurable increase in access to this advanced breast cancer screening—especially among underserved communities, according to a new UCLA study. Digital breast tomosynthesis, or 3D mammography, offers clearer images and fewer false positives than traditional methods. But even small out-of-pocket costs can deter patients from choosing it. After UCLA eliminated the fee in 2021, usage jumped from 83.7% to 91.5%. The gains were even more striking among historically marginalized groups. Asian, Black, and Hispanic women saw increases of 5.0, 6.2, and 6.2 percentage points respectively beyond the gains seen in white patients. Non-English speakers experienced a 7.1 percentage point greater increase than English-speaking patients. Medicaid recipients and those from lower-income areas also benefited more than average. “These findings demonstrate that even modest out-of-pocket costs can create meaningful barriers to accessing advanced screening technology,” said Dr. Nina M. Capiro, lead author and UCLA Health radiologist. She emphasized that while the fee removal helped, “persistent disparities indicate that additional approaches are needed.” The study used a difference-in-difference analysis to isolate the impact of the fee change across 13,284 women. All had access to both 2D and 3D mammography at the time of screening. Researchers say the results offer a model for evaluating how financial policies affect health equity. But they also caution that eliminating fees alone won’t erase disparities—more comprehensive strategies are needed. See: “Effect of Fee Removal on the Usage of Digital Breast Tomosynthesis to Minimize Healthcare Disparities” (June 19, 2025)

Pregnant women from minority groups with cancer face more complications
Pregnant women from racial and ethnic minority groups who are also battling cancer face significantly higher risks of complications, according to new research presented at the American Association for Cancer Research Annual Meeting 2025. The study, led by Dr. Duke Appiah of Texas Tech University Health Sciences Center, found that these women are more likely to experience adverse pregnancy outcomes—including hypertensive disorders, gestational diabetes, fetal growth restriction, preterm birth, and maternal mortality. “Maternal mortality was high among patients with cancer for all racial and ethnic groups,” Appiah said, “but the rates were even higher for minority women.” The study revealed that women with breast and thyroid cancer had a 30% elevated risk of complications, and that cancer itself significantly worsened outcomes even within the same racial group. Appiah pointed to preexisting conditions like hypertension and diabetes, as well as socioeconomic status and cancer treatments during pregnancy, as contributing factors. “Four in 10 women with cancer from racial and ethnic minority groups are likely to have one of the adverse pregnancy outcomes,” he noted. Current clinical guidelines are not comprehensive, leaving physicians to make decisions without robust data. Appiah’s team hopes their findings will help inform both patients and providers. “We are providing them with information to help them make more informed decisions,” he said. See: “Findings Reveal Gaps in Care for Pregnant Minority Women With Cancer” (June 19, 2025)

Discrimination, Police Violence Linked to Higher Risk of Psychotic Symptoms for People of Color
New research shows that systemic social factors—including racism and police violence—may heighten the risk of psychotic experiences among young adults of color in the United States. The study, published in Schizophrenia Bulletin, analyzed survey data from more than 1,500 individuals aged 18 to 29. The findings reveal sharp disparities. Young adults identifying as Black, Indigenous, or People of Color were 60% more likely to report psychotic experiences in the past year compared with their White peers. Those who experienced police violence were 52% more likely to report such symptoms. Everyday discrimination, substance use, and childhood abuse also increased the odds of reporting psychotic experiences. “These results suggest that reducing exposure to systemic factors, like societal racism, may provide mental health benefits similar to individual-focused interventions, like psychotherapy,” said coauthor Jordan E. DeVylder of New York University. The study adds to a growing body of evidence that mental health disparities are rooted not only in biology or individual behavior, but in broader social structures. For marginalized communities, the daily stress of discrimination and repeated exposure to violence can become risk factors as potent as clinical ones. Researchers conclude that mental health policy must account for systemic inequities. Addressing racism, policing practices, and social exclusion could help reduce the disproportionate burden of psychotic symptoms among minority youth. See: “Systemic Social Factors May Increase the Risk for Psychotic Experiences” (June 18, 2025)

Peer Support Boosts Black Breast Cancer Care
Digital coaching and peer navigation may improve outcomes for breast cancer survivors, particularly Black women who face stark disparities in care, according to a new study led led by Dr. Robin Lally and her team at the University of Nebraska Medical Center. The REALIZE study, co-led by Dr. Juan Santamaria, focuses on African American women, who are diagnosed with breast cancer at lower rates but experience a 40% higher mortality rate. Early findings suggest that pairing newly diagnosed patients with peer survivors from their own communities can build trust, improve communication with providers, and increase adherence to treatment. “Navigated women reported satisfaction with the program, which increased over time,” the team noted. Dr. Lally emphasized the importance of refining this model to promote health equity. Presenting at national conferences, her team highlighted how community-based navigation bridges clinical care and research, offering a promising path to reduce disparities in breast cancer outcomes. See: “Dr. Lally and team explore two studies for breast cancer survivors” (June 18, 2025)

Persistent racial and ethnic disparities in adolescent mental health care
A new national study reveals persistent racial and ethnic disparities in adolescent mental health care, particularly in access to outpatient, school-based, and telemental health services. Drawing on data from over 23,000 adolescents, researchers found that non-Hispanic White teens were significantly more likely to receive mental health treatment than their peers from minority backgrounds. Only 21.9% of non-Hispanic Black adolescents and 25.6% of Hispanic adolescents reported receiving any mental health visit, compared to 31.7% of White adolescents. The gap was even wider in telemental health, where just 8.1% of Asian, Hawaiian, or Pacific Islander adolescents accessed services, versus 17.0% of White adolescents. Prescription medication use followed a similar pattern. While 17.4% of White adolescents received psychotropic medications, the rate dropped to 7.9% for Black adolescents and 3.9% for Asian, Hawaiian, or Pacific Islander adolescents. These disparities persisted even after adjusting for income, insurance, and health status. Interestingly, support groups and peer support services showed little to no racial or ethnic differences in use. This suggests that community-based, non-clinical approaches may offer more equitable access points for mental health care. Among adolescents with a history of major depressive episodes, the disparities were even more pronounced. Black teens were 20.7 percentage points less likely than White peers to have had a mental health visit, and 20.1 percentage points less likely to receive medication. These findings underscore the urgent need to address systemic barriers and expand culturally responsive care for minority youth. See: “Racial and Ethnic Differences in Mental Health Service Use Among Adolescents” (June 18, 2025)